Abstract
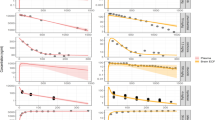
We attempted to predict the delivery of ofloxacin (OFLX), a new quinolone antibacterial agent (NQ), into cerebrospinal fluid (CSF) in the human based on the physiological properties and pharmacokinetic paramters of NQs in various animals. Physiological properties for evaluation of drug delivery into CSF such as volume and the bulk flow rate of CSF and weight of choroid plexus, were compared among the rat, rabbit, cat, dog, and human. Statistically significant correlations with power values of 0.82–0.89 in the linear regression were observed on log-log plots between brain weight and those properties of each species. Delivery of OFLX into CSF from blood was analyzed by “diffusion and flow model” with unidirectional efflux process from CSF to blood. The blood-CSF diffusion clearance and the efflux clearance of OFLX in the human were extrapolated from animal data based on the allometric correlations between brain weight and these parameters in the rat, rabbit, and dog. The apparent volume of distribution and the total body clearance of NQs in the human could also be predicted from animal data based on the classical Adolph-Dedrick approach. To simulate the CSF concentration-time profile of OFLX in the human by using these predicted parameters, it was necessary to consider both the lumbar CSF compartment and the ventricular CSF compartment. Both plasma and CSF concentration-time profiles of OFLX predicted from only animal experimental data were in good agreement with those observed clinically.
Similar content being viewed by others
References
E. E. Adolph. Quantitative relations in the physiological constitutions of mammals.Science 109:579–585 (1949).
R. L. Dedrick, D. D. Forester, J. N. Cannon, S. M. ElDareen, and L. B. Mellet. Pharmacokinetics of 1-β-D-arbino-furanoslycytosine (Ara-C) deamination in several species.Biochem. Pharmacol. 22:2405–2417 (1973).
R. L. Dedrick, K. B. Bischoff, and D. S. Zaharko. Interspecies correlation of plasma concentration history of methotrexate (NSC-740).Cancer Chemother. Rep. 54:95–101 (1970).
R. L. Dedrick, Animal scale-up.J. Pharmacokin. Biopharm. 1:435–461 (1973).
H. Boxenbaum. Interspecies scaling, allometry, physiological time, and the ground plan of pharmacokinetics.J. Pharmacokin. Biopharm. 10:201–227 (1982).
H. Boxenbaum. Comparative pharmacokinetics of benzodiazepines in dog and man.J. Pharmacokin. Biopharm. 10:411–426 (1982).
Y. Sawada, M. Hanano, Y. Sugiyama, and T. Iga. Prediction of the disposition of β-lactam antibiotics in humans from pharmacokinetic parameters in animals.J. Pharmacokin. Biopharm. 12:241–261 (1984).
Y. Sawada, M. Hanano, Y. Sugiyama, H. Harashima, and T. Iga. Prediction of the volumes of distribution of basic drugs in human based on data from animals.J. Pharmacokin. Biopharm. 12:587–596 (1984).
Y. Sawada, H. Harashima, M. Hanano, Y. Sugiyama, and T. Iga. Prediction of the plasma concentration time courses of various drugs in humans based on data from rats.J. Pharmacobio. Dyn. 8:757–766 (1985).
Y. Sawada, M. Hanano, Y. Sugiyama, and T. Iga. Prediction of the disposition of nine weakly acidic and six weakly basic drugs in humans from pharmacokinetic parameters in rats.J. Pharmacokin. Biopharm. 13:477–492 (1985).
R. L. Dedrick, E. H. Oldfield, and J. M. Collins. Arterial drug infusion with particular reference to the brain. Cancer Treat. Rep.68:373–380 (1984).
R. L. Dedrick. Interspecies scaling of regional drug delivery.J. Pharm. Sci. 75:1047–1052 (1986).
A. Ito, K. Hirai, M. Inoue, H. Koga, S. Suzue and S. Mitsuhashi.In vitro antibacterial activity of AM-715, a new nalidixic analog.Antimicrob. Agents Chemother. 17:103–108 (1980).
J. Matsumoto, T. Miyamoto, A. Minamida, Y. Nishimura, H. Egawa, and H. Nishimura. Structure-activity relationships of 4-oxo-1, 8-naphthyridine-3-carboxylic acids including AT-2266, a new oral antipseudomonal agent. In J. D. Nelson and C. Grassi (eds.),Current Chemotherapy and Infectious Disease, American Socity of Microbiology, Washington, DC, pp. 454–456 (1980).
K. Sato, Y. Matsuura, M. Inoue, T. Une, Y. Osada, H. Ogawa and S. Mitsuhashi.In vitro andin vivo activity of DL-8280, a new oxazine derivative,Antimicrob. Agents Chemother. 22:548–553 (1982).
R. Wise, J. M. Andrews, and L. J. Edwards.In vitro activity of BAY o 9867, a new quinolone derivative, compared with those of other antimicrobial agents.Antimicrob. Agents Chemother. 23:559–564 (1983).
R. Malinverni and M. P. Glauser. Comparative studies of fluoroquinolones in the treatment of urinary tract infections,Rev. Infect. Dis. 10 (Suppl. 1):S153-S163 (1988).
J.-P. Thys, Quinolones in the treatment of bronchopulmonary infections.Ref. Infect. Dis. 10(Suppl. 1):S212-S217 (1988).
J. H. Paton and D. S. Reeves. Clinical features and management of adverse effects of quinolone antibacterials.Drug Safety 6:8–27 (1991).
W. Christ, T. Lehnert, and B. Ulbrich. Specific toxicologic aspects of the quinolones.Ref. Infect. Dis. 10(Suppl. 1):S141-S146 (1988).
G. Takeo, N. Shibuya, M. Motomura, H. Kanazawa, and H. Shishido. A new DNA gyrase inhibitor induces convulsions: A case report and animal experiments.Chemotherapy (Tokyo)37:1154–1159 (1989).
J. H. Paton, and D. S. Reeves. Clinical features and management of adverse effects of quinolone antibacterials.Drug Safety 6:8–27 (1991).
H. Sato, E. Okezaki, S. Yamamoto, O. Nagata, H. Kato, and A. Tsuji. Entry of the new quinolone antibacterial agents of ofloxacin and NY-198 into the central nervous system in rats.J. Pharmacobiodyn. 11:386–394 (1988).
G. Valainis, D. Thomas, and G. Pankey. Penetration of ciprofloxacin into cerebrospinal fluid.Eur. J. Clin. Microbiol. 5:206–207 (1986).
J. B. McClain, J. Rhoads, and G. Krol. Cerebrospinal fluid concentrations of ciprofloxacin in subjects with uninflamed meninges.J. Antimicrob. Chemother. 21:808–809 (1988).
D. N. Gerding and J. A. Hitt. Tissue penetration of the new quinolones in humans.Rev. Infect. Dis. 11(Suppl. 5):S1046-S1057 (1989).
W. M. Scheld. Quinolone therapy for infections of the central nervous systemRev. Infect. Dis. 11(Suppl. 5):S1194-S1202 (1989).
K. Kawahara. Penetration of fluoroquinolones into human cerebrospinal fluid.Chemotherapy (Tokyo)38:461–476 (1990).
K. Kawahara, M. Kawahara, T. Goto and Y. Ohi. Penetration of sparfloxacin into the human spinal fluid: a comparative study with 5 other fluoroquinolones.Chemotherapy (Tokyo)39:(Suppl. 4):149–157 (1991).
T. V. Tho, A. Armengaud, and B. Davet. Diffusion of enoxacin into the cerebrospinal fluid in dogs with healthy meninges and with experimental meningitis.J. Antimicrob. Chemother. 14(Suppl. C):57–62 (1984).
F. Taga, F. Kobayashi, S. Saito, T. Ooie, F. Kawahara, H. Uchida, J. Simada, S. Hori, and O. Sakai. Possibility for induction of convulsion by fleroxacin and its disposition in the central nervous system.Arzneim. Forsch. 40:900–904 (1990).
N. Bitar, R. Claes, and P. V. der Auwera. Concentration of ofloxacin in serum and cerebrospinal fluid of patients without meningitis receiving the drug intravenously and orally.Antimicrob. Agents Chemother. 33:1686–1690 (1989).
M. Drancourt, H. Gallais, D. Raoult, E. Estrangin, M. N. Mallet, and P. de Micco. Ofloxacin penetration into cerebrospinal fluid.J. Antimicrob. Chemother. 22:263–265 (1988).
A. M. Shibl, C. J. Hackbarth, and M. A. Sande. Evaluation of pefloxacin in experimental Escherichia coli meningitis.Antimicrob. Agents Chemother. 29:409–411 (1986).
M. Neuman. Clinical pharmacokinetics of the newer antibacterial 4-quinolones.Clin. Pharmacokin.14:96–121 (1988).
J. Dow, J. Chazal, A. M. Frydman, R. Woehrle, F. Djebbar, and J. Gaillot. Transfer kinetics of pefloxacin into cerebro-spinal fluid after one hour iv infusion of 400 mg in man.J. Antimicrob. Chemother.17(Suppl. B):81–87 (1986).
K. Yamaoka, Y. Tanigawara, T. Nakagawa, and T. Uno. A pharmacokinetic analysis program (MULTI) for microcomputer.J. Pharmacobiodyn.4:879–885 (1981).
M. Gibaldi and D. Perrier. Drugs and the pharmaceutical sciences. In J. Swarbrick (ed.),Pharmacokinetics, Vol. 1, Marcel Dekker, New York, 1975.
M. D. Karol, P. V. Pedersen, and R. E. Brashear. Diffusion and flow transfer of theophylline across the blood-brain barrier: pharmacokinetic analysis.J. Pharmacokin. Biopharm. 11:273–287 (1983).
J. M. Collins and L. Dedrick. Distributed model for drug delivery to CSF and brain tissue.Am. J. Physiol. 245:R303-R310 (1983).
R. G. Blasbert, C. S. Patlak, and W. R. Shapiro. Distribution of methotrexate in the cerebrospinal fluid and brain and after intraventricular administration.Cancer Treat. Rep. 61:633–641 (1977).
W. R. Shapiro, D. F. Young, and B. M. Mehta. Methotrexate: Distribution in cerebrospinal fluid after intravenous, ventricular and lumbar injections.New Engl. J. Med. 293:161–166 (1975).
H. F. Cserr and B. J. Berman. Iodide and thiocyanate efflux from brain following injection into rat caudate nucleus.Am. J. Physiol. 235:F331-F337 (1978).
H. Cserr. Potassium exchange between cerebrospinal fluid, plasma, and brain.Am. J. Physiol. 209:1219–1226 (1965).
R. E. Harbut and C. E. Johanson. Third ventricle choroid plexus function and its response to acute perturbations in plasma chemistry.Brain Res.374:137–146 (1986).
M. Pollay and H. Davson. The passage of certain substances out of the cerebrospinal fluid.Brain 86:137–150 (1963).
K. Welch. Secretion of cerebrospinal fluid by choroid plexus of the rabbit.Am. J. Physiol. 205:617–624 (1963).
A. V. Lorenzo and S. R. Snodgrass. Leucine transport from the ventricles and the cranial subarachnoid space in the cat.J. Neurochem. 19:1287–1298 (1972).
R. Spector and A. V. Lorenzo. The transport and metabolism of salicylate in the central nervous system:in vivo studies.J. Pharmacol. Exp. Ther. 185:276–286 (1973).
S. R. Heisey, D. Held, and J. R. Pappenheimer. Bulk flow and diffusion in the cerebrospinal fluid system of the goat.Am. J. Physiol. 203:775–781 (1962).
E. A. Bering Jr. Circulation of the cerebrospinal fluid: demonstration of the choroid plexuses as the generator of the force for flow of fluid and ventricular enlargement.J. Neurosurg. 19:405–413 (1962).
A. Sahar. The effect of pressure on the production of cerebrospinal fluid by the choroid plexus.J. Neurol. Sci. 16:49–58 (1972).
W. W. Oppelt, T. H. Maren, E. S. Owens, and D. P. Rall. Effects of acid-base alterations on cerebrospinal fluid production.Proc. Soc. Exp. Biol. (N.Y.)114:86–89 (1963).
E. A. Bering Jr. Cerebrospinal fluid production and its relationship to cerebral metabolism and cerebral blood flow.Am. J. Physiol. 197:825–828 (1959).
P. L. Alyman and D. S. Dittmer (eds).Biology Data Book, 2nd ed., Vol. 3. Federation of American Societies for Experimental Biology, Bethesda, MD, 1974.
A. Tuji, H. Sato, Y. Kume, I. Tamai, E. Okezaki, O. Nagata, and H. Kato. Inhibitory effects of quinolone antibacterial agents on γ-aminobutyric acid binding to receptor sites in rat brain membranes.Antimicrob. Agents Chemother. 32:190–194 (1988).
S. Nakamura, N. Kurobe, S. Kashimoto, T. Ohue, Y. Takase, and M. Shimizu. Absorption distribution, excretion and metabolism of AT-2266 in experimental animals.Chemotherapy (Tokyo)32(Suppl. 3):86–84 (1984).
M. Kawai, M. Nakanishi and N. Maekawa. Phase I study of AT-2266.Chemotherapy (Tokyo)32(Suppl. 3):334–358 (1984).
E. Okezaki, K. Ohmishi, S. Koike, Y. Takahashi, and E. Makino. Disposition and metabolism of NY-198 I: bioassay study of absorption, distribution and excretion in various animals.Chemotherapy (Tokyo)36(Suppl. 2):132–137 (1988).
E. Okezaki, E. Makino, K. Ohmishi, O. Nagata, T. Yamada, and K. Takahashi. Disposition and metabolism of NY-198 II:HPLC and bioassay studies of absorption and excretion in dog.Chemotherapy (Tokyo)36(Suppl. 2):138–143 (1988).
O. Nagata, T. Yamada, K. Takahashi, E. Okezaki, T. Yanagida, and H. Nakanishi. Disposition and metabolism of NY-198 III: absorption, metabolism and excretion of NY-198 in monkeys by high-performance liquid chromatography.Chemotherapy (Tokyo)36(Suppl. 2):144–150 (1988).
O. Nagata, T. Yamada, T. Yamaguchi, E. Okezaki, T. Terasaki, and A. Tsuji. Disposition and metabolism of NY-198 IV: absorption, distribution and excretion of14C-NY-198 in rats and dogs.Chemotherapy (Tokyo)36(Suppl. 2):151–173 (1988).
M. Nakashima, T. Uematsu, Y. Takiguchi, A. Mizuno, and M. Kanamaru. Phase I study on NY-198.Chemotherapy, (Tokyo)36(Suppl. 2):201–239 (1988).
S. Murayama, K. Hirai, A. Ito, Y. Abe, and T. Irikura. Studies on absorption, distribution and excretion of AM-715 in animals by bioassay method.Chemotherapy (Tokyo)29(Suppl. 4):98–104 (1981).
Y. Nagatsu, K. Endo, and T. Irikura. Studies on the fate of14C-labelled AM-715Chemotherapy (Tokyo)29(Suppl. 4):105–118 (1981).
T. Abiko and A. Ishihama. Phase I study on AM-715.Chemotherapy (Tokyo)29(Suppl. 4):136–145 (1981).
M. Tsumura, K. Sato, T. Une, and H. Tachizawa. Metabolic disposition of DL-8280. The first report: comparison between absorption and excretion of DL-8280 in the dog and monkey by bioassay and HPLC methods.Chemotherapy (Tokyo)32(Suppl. 1):1179–1184 (1984).
O. Okazaki, T. Kurata, K. Hashimoto, K. Sudo, M. Tsumura, and H. Tachizawa. Metabolic disposition of DL-8280: The second report: Absorption, distribution and excretion of14C-DL-8280 in various animal species.Chemotherapy (Tokyo)32(Suppl. 1):1185–1202 (1984).
N. Ichihara. Phase I study on DL-8280.Chemotherapy (Tokyo)32(Suppl. 1):118–149 (1984).
G. Montay, Y. Goueffon, and F. Roquet. Absorption, distribution, metabolic fate, and elimination of pefloxacin mesylate in mice, rats, dogs, monkeys, and humans.Antimicrob. Agents Chemother. 25:463–472 (1984).
T. Yasuda, Y. Watanabe, T. Hayashi, and R. Kitayama. Serum protein binding of T-3262.Chemotherapy (Tokyo)36(Suppl. 9)143–148 (1988).
T. Yasuda, Y. Watanabe, S. Minami, K. Kumano, S. Takagi, R. Tsuneda, and J. Kanayama. Absorption, distribution, metabolism and excretion of T-3262 in experimental animals.Chemotherapy (Tokyo)36(Suppl. 9):149–157 (1988).
M. Nakashima, T. Uematsu, and M. Kanamaru. Phase I study of T-3262, a new pyridonecarboxylic acid derivative.Chemotherapy (Tokyo)36(Suppl. 9):158–180 (1988).
H. Lode, G. Hoffken, K. Borner, and P. Koeppe. Unique aspects of quinolone pharmacokinetics.Clin. Pharmacokin. 16(Suppl. 1):1–4 (1989).
A. M. Korinek, G. Montay, A. Bianchi, M. Guggiari, R. Grob, and P. Viars. Penetration of pefloxacin into human brain tissue.Rev. Infect. Dis. 10(Suppl. 1):S257 (1988).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kawakami, J., Yamamoto, K., Sawada, Y. et al. Prediction of brain delivery of ofloxacin, a new quinolone, in the human from animal data. Journal of Pharmacokinetics and Biopharmaceutics 22, 207–227 (1994). https://doi.org/10.1007/BF02353329
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF02353329