Abstract
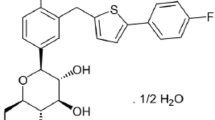
Sodium-glucose co-transporter 2 (SGLT2) is predominantly expressed in the S1 segment of the proximal tubule of the kidney and is the major transporter responsible for mediating renal glucose reabsorption. Dapagliflozin is an orally active, highly selective SGLT2 inhibitor that improves glycemic control in patients with type 2 diabetes mellitus (T2DM) by reducing renal glucose reabsorption leading to urinary glucose excretion (glucuresis). Orally administered dapagliflozin is rapidly absorbed generally achieving peak plasma concentrations within 2 h. Dose-proportional systemic exposure to dapagliflozin has been observed over a wide dose range (0.1–500 mg) with an oral bioavailability of 78 %. Dapagliflozin has extensive extravascular distribution (mean volume of distribution of 118 L). Dapagliflozin metabolism occurs predominantly in the liver and kidneys by uridine diphosphate-glucuronosyltransferase-1A9 to the major metabolite dapagliflozin 3-O-glucuronide (this metabolite is not an SGLT2 inhibitor at clinically relevant exposures). Dapagliflozin is not appreciably cleared by renal excretion (<2 % of dose is recovered in urine as parent). Dapagliflozin 3-O-glucuronide elimination occurs mainly via renal excretion, with 61 % of a dapagliflozin dose being recovered as this metabolite in urine. The half-life for orally administered dapagliflozin 10 mg was 12.9 h. Maximal increases in urinary glucose excretion were seen at doses ≥20 mg/day in patients with T2DM. No clinically relevant differences were observed in dapagliflozin exposure with respect to age, race, sex, body weight, food, or presence of T2DM. Pharmacodynamic changes are dependent on plasma glucose and renal function, and decreases in urinary glucose excretion were observed due to the lower filtered load (plasma glucose × glomerular filtration rate) in healthy volunteers compared to subjects with T2DM. After multiple doses of dapagliflozin, urinary glucose excretion was associated with dose-related decreases in plasma glucose parameters in subjects with T2DM. Patients with severe renal or hepatic impairment show higher systemic exposure to dapagliflozin. No clinically relevant drug interactions were observed that would necessitate dose adjustment of dapagliflozin when administered with other antidiabetic or cardiovascular medications, as well as drugs that could potentially influence dapagliflozin metabolism.



Similar content being viewed by others
References
International Diabetes Foundation. The global burden. International Diabetes Foundation Web site. http://www.diabetesatlas.org/book/export/html/36. Accessed 4 Mar 2013.
World Diabetes Foundation. Diabetes facts. World Diabetes Foundation Web site. http://www.worlddiabetesfoundation.org/composite-35.html. Accessed 4 Mar 2013.
World Health Organisation. Global strategy on diet, physical activity and health. World Health Organisation Web site. http://www.who.int/dietphysicalactivity/publications/facts/obesity/en/. Accessed 4 Mar 2013.
American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36:S11–66.
Braga MF, Casanova A, Teoh H, et al. Poor achievement of guidelines-recommended targets in type 2 diabetes: findings from a contemporary prospective cohort study. Int J Clin Pract. 2012;66:457–64.
Hermans MP, Brotons C, Elisaf M, et al. Optimal type 2 diabetes mellitus management: the randomised controlled OPTIMISE benchmarking study: baseline results from six European countries. Eur J Prev Cardiol. 2012. doi:10.1177/2047487312449414.
Wong ND, Glovaci D, Wong K, et al. Global cardiovascular disease risk assessment in United States adults with diabetes. Diab Vasc Dis Res. 2012;9:146–52.
Marsenic O. Glucose control by the kidney: an emerging target in diabetes. Am J Kidney Dis. 2009;53:875–83.
Kim Y, Babu AR. Clinical potential of sodium-glucose cotransporter 2 inhibitors in the management of type 2 diabetes. Diabetes Metab Syndr Obes. 2012;5:313–27.
Meng W, Ellsworth BA, Nirschl AA, et al. Discovery of dapagliflozin: a potent, selective renal sodium-dependent glucose cotransporter 2 (SGLT2) inhibitor for the treatment of type 2 diabetes. J Med Chem. 2008;51:1145–9.
Ferrannini E, Ramos SJ, Salsali A, et al. Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: a randomized, double-blind, placebo-controlled, phase 3 trial. Diabetes Care. 2010;33:2217–24.
List JF, Woo V, Morales E, et al. Sodium-glucose cotransport inhibition with dapagliflozin in type 2 diabetes. Diabetes Care. 2009;32:650–7.
Bailey CJ, Gross JL, Pieters A, et al. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;375:2223–33.
Wilding JP, Norwood P, T’joen C, et al. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers: applicability of a novel insulin-independent treatment. Diabetes Care. 2009;32:1656–62.
Ptaszynska A, Johnsson K, Apanovitch A, et al. Safety of dapagliflozin in clinical trials for T2DM. Diabetes. 2012;61(suppl 1):A258–9.
Boulton DW, Kasichayanula S, Keung CF, et al. Simultaneous oral therapeutic and intravenous (1)(4)C-microdoses to determine the absolute oral bioavailability of saxagliptin and dapagliflozin. Br J Clin Pharmacol. 2013;75:763–8.
Obermeier M, Yao M, Khanna A, et al. In vitro characterization and pharmacokinetics of dapagliflozin (BMS-512148), a potent sodium-glucose cotransporter type II inhibitor, in animals and humans. Drug Metab Dispos. 2010;38:405–14.
Zinker B, Ma X, Liu H, et al. Chronic dapagliflozin treatment reduces elevated hepatic glucose production and enhances pancreatic insulin content in male ZDF rats. (Abstract 1031-P). Diabetes. 2011;60(suppl 1):A283.
Forxiga: Summary of Product Characteristics. AstraZeneca and Bristol-Myers Squibb. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002322/WC500136026.pdf. Accessed 8 Apr 2013.
Kasichayanula S, Liu X, Zhang W, et al. Effect of a high-fat meal on the pharmacokinetics of dapagliflozin, a selective SGLT2 inhibitor, in healthy subjects. Diabetes Obes Metab. 2011;13:770–3.
Kasichayanula S, Liu X, Zhang W, et al. Influence of hepatic impairment on the pharmacokinetics and safety profile of dapagliflozin: an open-label, parallel-group, single-dose study. Clin Ther. 2011;33:1798–808.
Kasichayanula S, Liu X, Benito MP, et al. The influence of kidney function on dapagliflozin exposure, metabolism, and efficacy in healthy subjects and in patients with type 2 diabetes mellitus. Br J Clin Pharmacol. 2013;76(3):432–44. doi:10.1111/bcp.12056.
Kasichayanula S, Yao M, Vachharajani M, et al. Disposition and Mass Balance of [14C]-dapagliflozin after single oral dose in healthy male volunteers. AAPS J. 2008;10(S2).
Dostalek M, Court MH, Hazarika S, et al. Diabetes mellitus reduces activity of human UDP-glucuronosyltransferase 2B7 in liver and kidney leading to decreased formation of mycophenolic acid acyl-glucuronide metabolite. Drug Metab Dispos. 2011;39:448–55.
Abdul-Ghani MA, DeFronzo RA. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocr Pract. 2008;14:782–90.
Vallon V, Platt KA, Cunard R, et al. SGLT2 mediates glucose reabsorption in the early proximal tubule. J Am Soc Nephrol. 2011;22:104–12.
Wright EM, Loo DD, Hirayama BA. Biology of human sodium glucose transporters. Physiol Rev. 2011;91:733–94.
Hummel CS, Lu C, Liu J, et al. Structural selectivity of human SGLT inhibitors. Am J Physiol Cell Physiol. 2012;302:C373–82.
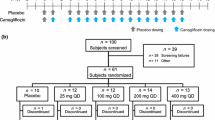
Komoroski B, Vachharajani N, Feng Y, et al. Dapagliflozin, a novel, selective SGLT2 inhibitor, improved glycemic control over 2 weeks in patients with type 2 diabetes mellitus. Clin Pharmacol Ther. 2009;85:513–9.
DeFronzo RA, Hompesch M, Kasichayanula S, et al. Characterization of renal glucose reabsorption in response to dapagliflozin in healthy subjects and subjects with type 2 diabetes. Diabetes Care. 2013 [Epub ahead of print].
Komoroski B, Vachharajani N, Boulton D, et al. Dapagliflozin, a novel SGLT2 inhibitor, induces dose-dependent glucosuria in healthy subjects. Clin Pharmacol Ther. 2009;85:520–6.
Carlson GF, Tou CK, Parikh S, et al. Evaluation of the effect of dapagliflozin on cardiac repolarization: a thorough QT/QTc study. Diabetes Ther. 2011;2:123–32.
Kasichayanula S, Chang M, Hasegawa M, et al. Pharmacokinetics and pharmacodynamics of dapagliflozin, a novel selective inhibitor of sodium-glucose co-transporter type 2, in Japanese subjects without and with type 2 diabetes mellitus. Diabetes Obes Metab. 2011;13:357–65.
Yang L, Li H, Li H, et al. Pharmacokinetic and pharmacodynamic properties of single- and multiple-dose of dapagliflozin, a selective inhibitor of SGLT2, in healthy Chinese subjects. Clin Ther. 2013;35(8):1211–22.e2.
Kasichayanula S, Liu X, Shyu WC, et al. Lack of pharmacokinetic interaction between dapagliflozin, a novel sodium-glucose transporter 2 inhibitor, and metformin, pioglitazone, glimepiride or sitagliptin in healthy subjects. Diabetes Obes Metab. 2011;13:47–54.
Imamura A, Kusunoki M, Ueda S, et al. Impact of voglibose on the pharmacokinetics of dapagliflozin in Japanese patients with type 2 diabetes. Diabetes Ther. 2013;4(1):41–9.
Kasichayanula S, Chang M, Liu X, et al. Lack of pharmacokinetic interactions between dapagliflozin and simvastatin, valsartan, warfarin, or digoxin. Adv Ther. 2012;29:163–77.
Wilcox CS, Liu X, Kasichayanula S, et al. Evaluation of interactions of dapagliflozin and bumetanide. Presented at: American Society of Nephrology, Denver (2010).
Kasichayanula S, Liu X, Griffen SC, et al. Effects of rifampin and mefenamic acid on the pharmacokinetics and pharmacodynamics of dapagliflozin. Diabetes Obes Metab. 2013;15:280–3.
Acknowledgments
Medical writing assistance was provided by Ray Ashton and Karen Pemberton, PhD of PPSI (a PAREXEL company) and was funded by AstraZeneca and Bristol-Myers Squibb. All authors are employees of Bristol-Myers Squibb.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kasichayanula, S., Liu, X., LaCreta, F. et al. Clinical Pharmacokinetics and Pharmacodynamics of Dapagliflozin, a Selective Inhibitor of Sodium-Glucose Co-transporter Type 2. Clin Pharmacokinet 53, 17–27 (2014). https://doi.org/10.1007/s40262-013-0104-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-013-0104-3