Abstract
Purpose. A combination of proton pump inhibitors and antimicrobials has been applied as an anti–Helicobacter pylori (H. pylori) therapy. Omeprazole, one of the proton pump inhibitors, is metabolized by CYP2C19, which exhibits genetic polymorphism. It was reported previously that the overall anti–H. pylori efficacy can be related to the CYP2C19 genotype. The main aim of the present study was to obtain a rational explanation for the relationship between the overall anti–H. pylori efficacy and the CYP2C19 genotype.
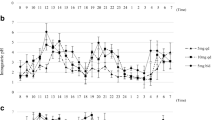
Methods. Six healthy volunteers were classified as extensive metabolizers and poor metabolizers, according to their CYP2C19 genotypes. Plasma concentrations and intragastric pH were monitored prior to and until 24 h after the administration of 20 mg omeprazole. The stability of amoxicillin, clarithromycin, and metronidazole was examined using buffer solutions with monitored intragastric pH, and their remaining percentage in the intragastric space was simulated.
Results. The poor metabolizers, classified by the CYP2C19 genotypes, showed the higher effectiveness in anti–H. pylori therapy, via the higher plasma concentration of omeprazole and the higher intragastric pH, and possibly the higher stability of antimicrobials in the higher intragastric pH.
Conclusions. CYP2C19 genotyping is a very useful method to determine the effective and safe dosage regimen including the selection of the dual and triple therapy in anti–H. pylori therapy.
Similar content being viewed by others
REFERENCES
U. A. Meyer and U. M. Zanger. Molecular mechanisms of genetic polymorphisms of drug metabolism. Annu. Rev. Pharmacol. Toxicol. 137:269–296 (1997).
K. Brosen, S. M. F. de Morais, U. A. Meyer, and J. A. Goldstein. A multifamily study on the relationship between CYP2C19 genotype and S–mephenytoin oxidation phenotype. Pharmacogenetics 5:312–317 (1995).
L. Bertisson. Geographical/Interracial differences in polymorphic drug oxidation: Current state of knowledge of cytochromes P450 (CYP) 2D6 and 2C19. Clin. Pharmacokinet. 29:192–209 (1995).
J. D. Balian, N. Sukhova, J. W. Haris, et al. The hydroxylation of omeprazole correlates with S–mephenytoin metabolism: a population study. Clin. Pharmacol. Ther. 57:662–669 (1995).
S. M. F. de Morais, G. R. Wilkinson, J. Blaisdell, K. Nakamura, U. A. Meyer, and J. A. Goldstein. The major genetic defect responsible for the polymorphism of S–mephenytoin metabolism in humans. J. Biol. Chem. 269:15419–25422 (1994).
S. M. F. de Morais, G. R. Wilkinson, J. Blaisdell, U. A. Meyer, K. Nakamura, and J. A. Goldstein. Identification of a new genetic defect responsible for the polymorphism of S–mephenytoin metabolism in Japanese. Mol. Pharmacol. 46:594–598 (1994).
I. Ieiri, T. Kubota, A. Urae, et al. Pharmacokinetics of omeprazole (a subtrate of CYP2C19) and comparison with two mutant alleles, CYP2C19m1 in exon 5 and CYP2C19m2 in exon 4, in Japanese subjects. Clin. Pharmacol. Ther. 59:647–53 (1996).
T. Kubota, K. Chiba, and T. Ishizaki. Genotyping of S–mephenytoin 4′–hydroxylation in an extended Japanese population. Clin. Pharmacol. Ther. 60:661–666 (1996).
G. R. Deng. A sensitive non–radioactive PCR–RFLP analysis for detecting point mutation at 12th codon of oncogene c–Ha–ras in DNAs of gastric cancer. Nucleic Acids Res. 16:6231 (1988).
K. Okumura, T. Kita, S. Chikazawa, F. Komada, S. Iwakawa, and Y. Tanigawara. Genotyping of N–acetylation polymorphism and correlation with procainamide metabolism. Clin. Pharmacol. Ther. 61:509–517 (1997).
C. W. Howden. Clinical pharmacology of omeprazole. Clin. Pharmacokinet. 20:38–49 (1991).
E. Bayerdorffer, S. Miehlke, G. A. Mannes, et al. Double–blind trial of omeprazole and amoxicillin to cure Helicobacter pylori Infection in patients with duodenal ulcer. Gastroenterology 108:1412–1417 (1995).
T. Lind, F. Megraud, P. Unge, E. et al. The MACH2 study: Role of omeprazole in eradication of Helicobacter pylori with 1–week triple therapies. Gastroenterology 116:248–253 (1999).
J. Labenz, E. Gyenes, G. H. Ruhl, and G. Borsch. Amoxicillin plus omeprazole versus triple therapy for eradication of Helicobacter pylori in duodenal ulcer disease: A prospective, randomised and controlled study. Gut 34:1167–1170 (1993).
G. N. J. Tytgat. Review article: Treatments that impact favourably upon the eradication of Helicobacter pylori and ulcer recurrence. Aliment. Pharmacol. Ther. 8:359–368 (1994).
J. S. Dixon. Helicobacter pylori eradication: Unravelling the facts. Scand. J. Gastroenterology 30:48–62 (1995).
T. Lind, Z. S. van Veldhuyzen, R. Unge, et al. Eradication of Helicobacter pylori using one–week triple therapies combining omeprazole with two antimicrobials: The MACH 1 study. Helicobacter 1:138–144 (1996).
G. Cederbrant, G. Kahlmeter, C. Schalen, and C. Kamme. Additive effect of clarithromycin combined with 14–hydroxy clarithromycin, erythromicin, amoxicillin, metronidazole or omeprazole against Helicobacter pylori. J. Antimicrob. Chemother. 34:1025–1029 (1994).
Y. J. Debets–Ossenkopp, F. Namavar, and D. M. MacLaren. Effect of an acidic environment on the susceptibility of Helicobacter pylori to trospectomycin and other antimicrobial agents. Eur. J. Clin. Microbiol. Infect. Dis. 14:353–355 (1995).
D. Scott, D. Weeks, K. Melchers, and G. Sachs. The life and death of Helicobacter pylori. Gut 43:S56–S60 (1998).
A. F. Goddard, M. J. Jessa, D. A. Barret, et al. Effect of omeprazole on the distribution of metronidazole, amoxicillin, and clarithromycin in human gastric juice. Gastroenterology 111:358–367 (1996).
L. E. Gustavon, J. F. Kaiser, A. L. Edmonds, C. S. Locke, M. L. DeBartolo, and D. W. Schneck. Effect of omeprazole on concentrations of clarithromycin in plasma and gastric tissue at steady state. Antimicrob. Agents Chemother. 39:2078–2083 (1995).
P. O. Erah, A. F. Goddard, D. A. Barrett, P. N. Shaw, and R. C. Spiller. The stability of amoxicillin, clarithromycin and metronidazole in gastric juice: Relevance to the treatment of Helicobacter pylori infection. J. Antimicrob. Chemother. 39:5–12 (1997).
D. R. Sohn, K. Kobayashi, K. Chiba, K. H. Lee, S. G. Shin, and T. Ishizaki. Disposition kinetics and metabolism of omeprazole in extensive and poor metaolizers of S–mephenytoin 4′–hydroxylation recruited from an Oriental population. J. Pharmacol. Exp. Ther. 262:1195–1202 (1992).
Y. Tanigawara, N. Aoyama, T. Kita, et al. CYP2C19 genotype–related efficacy of omeprazole for the treatment of infection caused by Helicobacter pylori. Clin. Pharmacol. Ther. 66:528–534 (1999).
N. Aoyama, Y. Tanigawara, T. Kita, et al. Suffucuent effect of 1–week omeprazole and amoxicillin dual treatment for Helicobacter pylori eradication in cytochrome P450 2C19 poor metabolizers. J. Gastroenterol. 34:80–83 (1999).
T. Furuta, K. Ohashi, T. Kamata, M. Takashima, K. Kosuge, T. Kawasaki, et al. Effect of genetic differences in omeprazole metabolism on cure rates for Helicobacter pylori infection and peptic ulcer. Ann. Int. Med. 129:1027–1030 (1998).
K. Kobayashi. Simultaneous determination of omeprazole and its metabolites in plasma and urine by reversed–phase high–performance liquid chromatography with an alkaline–resistant polymer–coated C18 column. J. Chromatogra. 579:299–305 (1992).
J. Labenz, M. Stolte, A. L. Blum, et al. Intragastric acidity as a predictor of the success of Helicobacter pylori eradication: A study in peptic ulcer patients with omeprazole and amoxicillin. Gut 37:39–43 (1995).
A. Sjostedt, M. Sagar, G. Lindberg, B. Wikstrom, C. E. Nord, and R. Seensalu. Prolonged and profound acid inhibition is crucial in Helicobacter pylori treatment with a proton pump inhibitor combined with amoxicillin. Scand. J. Gastroenterology 33:39–43 (1998).
Y. J. Debets–Ossenkopp, S M parrius, J. G. Kusters, J. J. Kolkman, and C. M. J. E. Vandenbroucke–Grauls. Mechanism of clarithromycin resistance in clinical isolates of Helicobacter pylori. FEMS Microbiol. Lett. 142:37–42 (1996).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kita, T., Tanigawara, Y., Aoyama, N. et al. CYP2C19 Genotype Related Effect of Omeprazole on Intragastric pH and Antimicrobial Stability. Pharm Res 18, 615–621 (2001). https://doi.org/10.1023/A:1011025125163
Issue Date:
DOI: https://doi.org/10.1023/A:1011025125163