Abstract
The erythromycin breath test (EBT) is a putative probe of cytochrome P450 (CYP) 3A4 activity in vivo. Therefore, the EBT might prove useful for the individualisation of doses of drugs that have a low therapeutic window (for example the immunosuppressants or cytotoxics) and are metabolised by CYP3A4. However, there is a lack of consensus as to how the EBT should be used to predict total body clearance (CL), and the results so far have been largely disappointing.
We argue that the required assumption that individuals produce 5 mmol of CO2/min per m2 at rest is one of the problems with the existing EBT, as the literature suggests significant variability and possible gender differences in this parameter. An examination of the EBT with a simple compartment model suggests that alternative parameters could be more useful in the prediction of CL. In particular, there is theoretical support for the use of the time-point at which breath radioactivity is maximal (tmax) as a correlate for CL. This is in agreement with our recent study of the pharmacokinetics of erythromycin in patients with cancer.





Similar content being viewed by others
References
Wilkinson G. Cytochrome P4503A (CYP3A) metabolism: prediction of in vivo activity in humans. J Pharmacokinet Biopharm 1996; 24: 475–90
Watkins PB, Murray SA, Winkelman LG, et al. Erythromycin breath test as an assay of glucocorticoid-inducible liver cytochromes P-450. Studies in rats and patients. J Clin Invest 1989; 83: 688–97
Cheng CL, Smith DE, Carver PL, et al. Steady-state pharmaco-kinetics of delavirdine in HIV-positive patients: effect on erythromycin breath test [see comments]. Clin Pharmacol Ther 1997; 61: 531–43
Gharaibeh MN, Gillen LP, Osborne B, et al. Effect of multiple doses of rifampin on the [14C N-methyl]erythromycin breath test in healthy male volunteers. J Clin Pharmacol 1998; 38: 492–5
Kinirons MT, Krivoruk Y, Wilkinson GR, et al. Effects of ketoconazole on the erythromycin breath test and the dapsone recovery ratio [letter]. Br J Clin Pharmacol 1999; 47: 223–5
Polk RE, Crouch MA, Israel DS, et al. Pharmacokinetic interaction between ketoconazole and amprenavir after single doses in healthy men. Pharmacotherapy 1999; 19: 1378–84
Lane EA, Parashos I. Drug pharmacokinetics and the carbon dioxide breath test. J Pharmacokinet Biopharm 1986; 14: 29–49
Wagner D. CYP3A4 and the erythromycin breath test [letter]. Clin Pharmacol Ther 1998; 64: 129–30
Watkins PB. Noninvasive tests of CYP3A enzymes. Pharmacogenetics 1994; 4: 171–84
Hirth J, Watkins P, Strawderman M, et al. The effect of an individual’ cytochrome CYP3A4 activity on docetaxel clearance. Clin Cancer Res 2000; 6: 1255–8
Lan LB, Dalton JT, Schuetz EG. Mdrl limits CYP3A metabolism in vivo. Mol Pharmacol 2000; 58: 863–9
Krecic Shepard ME, Barnas CR, Slimko J, et al. In vivo comparison of putative probes of CYP3A4/5 activity: erythromycin, dextromethorphan, and Verapamil. Clin Pharmacol Ther 1999; 66: 40–50
Echizen H, Eichelbaum M. Clinical pharmacokinetics of Verapamil, nifedipine and diltiazem. Clin Pharmacokinet 1986; 11:425–49
Austin KL, Mather LE, Philpot CR, et al. Intersubject and doserelated variability after intravenous administration of erythromycin. Br J Clin Pharmacol 1980; 10: 273–9
Lown KS, Thummel KE, Benedict PE, et al. The erythromycin breath test predicts the clearance of midazolam. Clin Pharmacol Ther 1995; 57: 16–24
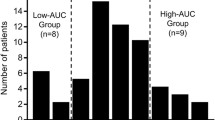
Rivory LP, Slaviero K, Seale JP, et al. Optimizing the erythromycin breath test for use in cancer patients. Clin Cancer Res 2000; 6: 3480–5
Krivoruk Y, Kinirons MT, Wood AJ, et al. Metabolism of cytochrome P4503A substrates in vivo administered by the same route: lack of correlation between alfentanil clearance and erythromycin breath test. Clin Pharmacol Ther 1994; 56: 608–14
Kinirons M, O’shea D, Kim RB, et al. Failure of erythromycin breath test to correlate with midazolam clearance as a probe of cytochrome P4503A. Clin Pharmacol Ther 1999; 66: 224–31
Kallie RN, Shreeve WW, Joubert SM. Studies in primary hyperuricaemia. 3. The conversion of 14C to breath 14CO2 from glucose-l-14C and glucose-6-14C in hyperuricaemia and gout. S Afr Med J 1968; 42: 473–6
Long CL, Nelson KM, Akin Jr JM, et al. Aphysiologic basis for the provision of fuel mixtures in normal and stressed patients. J Trauma 1990; 30: 1077–85
Legaspi A, Jeevanandam M, Starnes Jr HF, et al. Whole body lipid and energy metabolism in the cancer patient. Metabolism 1987; 36: 958–63
Shreeve WW, Cerasi E, Luft R. Metabolism of [2-14C]pyruvate in normal, acromegalic and HGH-treated human subjects. Acta Endocrinol Copenh 1970; 65: 155–69
Du Bois D, Du Bois E. A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med 1916; 17:863–71
Krecic Shepard ME, Barnas CR, Slimko J, et al. Gender-specific effects on Verapamil pharmacokinetics and pharmacodynamics in humans. J Clin Pharmacol 2000; 40: 219–30
Hunt CM, Westerkam WR, Stave GM, et al. Hepatic cytochrome P-4503A (CYP3A) activity in the elderly. Mech Ageing Dev 1992; 64: 189–99
Hunt CM, Westerkam WR, Stave GM. Effect of age and gender on the activity of human hepatic CYP3A. Biochem Pharmacol 1992; 44: 275–83
Cunningham JJ. Body composition and resting metabolic rate: the myth of feminine metabolism. Am J Clin Nutr 1982; 36: 721–6
Mao JC, Tardrew PL. Demethylation of erythromycins by rabbit tissues in vitro. Biochem Pharmacol 1965; 14: 1049–58
Irving CS, Schoeller DA, Nakamura KI, et al. The aminopyrine breath test as a measure of liver function. A quantitative description of its metabolic basis in normal subjects. J Lab Clin Med 1982; 100: 356–73
Riley RJ, Howbrook D. In vitro analysis of the activity of the major human hepatic CYP enzyme (CYP3A4) using [N-methyl-14C]-erythromycin. J Pharmacol Toxicol Methods 1997; 38: 189–93
Iwatsubo T, Hirota N, Ooie T, et al. Prediction of in vivo drug metabolism in the human liver from in vitro metabolism data. Pharmacol Ther 1997; 73: 147–71
Slaviero K. Validation of the erythromycin breath-test in cancer patients [honours thesis]. Sydney: University of Sydney, 1999
Acknowledgements
Supported by a grant from the New South Wales Cancer Council. This project was an initiative of the Pharmacology Interest Group of the Sydney Cancer Centre.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Consider the 1-compartment model illustrated in appendix figure 1 The concentrations of [14C]erythromycin (C) and formaldehyde product (M) are described by the differential equations:
A 1-compartment model to describe the concentrations of erythromycin (C), the formaldehyde intermediate (M) and the flux of CO2 following the administration of the erythromycin breath test (EBT). The cytochrome P450 (CYP) 3A4-mediated clearance of erythromycin is represented by the product of unbound fraction (fu) and intrinsic hepatic clearance (CLint), the balance of the total body clearance is indicated as CLother, and CLM is the total body clearance of the metabolite.
in which CLother is the balance of the total clearance (CL) not due to CYP3A4-mediated metabolism (i.e. CL = CLint · fu + CLother). The flux of CO2 at time t, CER(t), is usually expressed as a percentage of the dose. It follows that:
Substituting the solution for M from the differential equations yields:
This equation is similar to those proposed by Lown et al.[15] and Lane and Parashos.[7]
Integration of the area under the flux curve to infinity yields:
At the tmax of the breath flux versus time profile (equation 4), dCER/dt = 0 and, therefore:
Note the loss of the CLint term from this relationship. This underscores the fact that this novel parameter is unlikely to correlate with CYP3A4 activity per se unless, of course, this activity is the principal factor in determining CL.
Rights and permissions
About this article
Cite this article
Rivory, L.P., Slaviero, K.A., Hoskins, J.M. et al. The Erythromycin Breath Test For the Prediction of Drug Clearance. Clin Pharmacokinet 40, 151–158 (2001). https://doi.org/10.2165/00003088-200140030-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200140030-00001