Abstract
Linezolid is the first antibacterial to be approved from the oxazolidinone class. The drug has substantial antimicrobial activity against Gram-positive organisms such as streptococci, staphylococci and enterococci, including species resistant to conventional antibacterial treatment.
Linezolid is fully bioavailable following oral administration when compared with intravenous administration. Maximum plasma linezolid concentrations are usually achieved between 1 and 2 hours after oral administration. Food slightly decreases the rate, but not the extent, of absorption. The distribution of linezolid is approximately equivalent to total body water, and there is low protein binding (31%) to serum albumin.
The elimination half-life of linezolid is 5–7 hours, and twice-daily administration of 400–600mg provides steady-state concentrations in the therapeutic range. Linezolid is mainly cleared by non-renal clearance to two metabolites and renal clearance of the parent compound. Approximately 50% of an administered dose appears in the urine as the two major metabolites, and approximately 35% appears as parent drug. A small degree of nonlinearity has been observed, with a 30% decrease in clearance after a 5-fold increase in dose. The nonlinearity is not relevant over the therapeutic dosage range.
Plasma linezolid concentrations in elderly patients, patients with mild to moderate hepatic impairment or mild to severe renal impairment are similar to those achieved in young or healthy volunteers. Higher concentrations are observed in women as compared with men, but the difference is not sufficient to warrant an adjustment in dosage. In patients with severe renal impairment requiring haemodialysis, the exposure to the two primary metabolites was 7 to 8-fold higher than in patients with normal renal function. Therefore, linezolid should be used with caution in patients with severe renal insufficiency. A higher clearance of linezolid was found in children as compared with adults, and therefore higher daily dosages per kg bodyweight are required in children.
There is no pharmacokinetic interaction when linezolid is coadministered with aztreonam, gentamicin or warfarin. Linezolid is a mild, reversible, inhibitor of monoamine oxidases A and B. Coadministration of linezolid with the adrenergic agents pseudoephedrine and phenylpropanolamine resulted in increases in blood pressure relative to these agents alone or to placebo. The degree of the change in blood pressure was within that associated with normal daily activities. No interaction was observed when linezolid was coadministered with the serotonergic agent dextromethorphan.
Similar content being viewed by others
Linezolid is the first oxazolidinone antibacterial to be approved in the US and other countries throughout the world; it is available in both intravenous and oral dosage forms. The drug has substantial antimicrobial activity against Gram-positive bacteria such as staphylococci, streptococci and enterococci. Nominal 90% minimum inhibitory concentration (MIC90) values for target pathogens are 4, 2 and 1 mg/L for staphylococci, enterococci and streptococci, respectively. This includes activity against methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE).[1–5] Linezolid uniquely inhibits the formation of the bacterial protein synthesis initiation complex, possibly by distorting the binding site for initiator tRNA.[6,7] Crossresistance with linezolid has not been demonstrated in bacterial strains resistant to available antimicrobial agents, including other protein synthesis inhibitors.[5,8,9] Linezolid 400–600mg twice daily has demonstrated clinical efficacy in serious Gram-positive infections, including hospital- and community-acquired pneumonia, skin and soft tissue infections, and infections caused by MRSA and VRE, comparable with that of other antimicrobial agents with similar spectra of activity.[10–15]
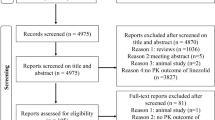
This report describes and reviews the available data pertaining to the pharmacokinetics of linezolid.
1. Pharmacokinetic Profile
The pharmacokinetics of linezolid have been assessed in healthy male and female volunteers following oral and intravenous administration. The following regimens have been assessed: single oral doses of 50–500mg;[16] multiple oral doses of 100–625mg given every 8 hours for up to 10 days;[16] multiple oral doses of 375–625mg given every 12 hours for 14 days;[17] single intravenous doses (30-minute infusion) of 250–750mg;[16] multiple intravenous doses of 250–500mg given every 8 hours for up to 7 days;[16] and multiple intravenous doses of 500 and 625mg given every 12 hours for 7 days.[17]
Linezolid has been approved as 400mg or 600mg administered twice daily. Doses of 375mg and 625mg were assessed in early pharmacokinetic trials, which approximate the final doses of 400mg and 600mg. A summary of the pharmacokinetic parameter values of linezolid in healthy volunteers after a single dose or multiple doses every 12 hours is provided in table I. Pharmacokinetic steady state is achieved after two to four doses of linezolid. The average steady-state minimum plasma concentrations (Cmin) were 3.9 and 8.02 mg/L for the 375mg and 625mg oral doses, respectively; the corresponding average maximum plasma concentrations (Cmax) were 13.2 and 18.8 mg/L, respectively.[17] Mean linezolid plasma concentrations are near or exceed the MIC90 values for the target pathogens for the entire 12-hour administration interval after oral or intravenous administration of 625mg.[17] Mean steady-state concentration-time profiles for oral linezolid 375mg and 625mg given twice daily are shown in figure 1.
Mean steady-state concentration-time profiles for oral linezolid 375 and 625mg every 12 hours.[17] Values are means α SD (n = 16).
In a study of dose proportionality after single and multiple doses from 125mg up to 625mg twice daily, a small degree of nonlinearity was observed, with a 30% decrease in clearance with a 5-fold increase in dose. After multiple doses, the clearance decreased about 10% relative to the single-dose estimates. Spectroscopy of urine showed that the major contributor to rate-limiting nonrenal clearance of linezolid was the formation of the major metabolite PNU-142586.[20] The degree of disproportionality is small relative to the overall degree of variability among subjects, and does not occur to any relevant degree over the therapeutic range of 400–600mg twice daily.[17,20]
The pharmacodynamics of linezolid have been investigated through the clinical outcome and pharmacokinetic results of phase II trials. The AUC/MIC ratio and/or Time above MIC were shown to be related to efficacy; as the AUC/MIC ratio and/or Time above MIC increased, so did the probability of efficacy or microbial eradication.[21,22] The demonstration of this relatedness does not eliminate the potential for other pharmacodynamic parameters to be predictive of efficacy, and numerous other host and infection factors may play a role in efficacy. No data are available that correlate adverse events or laboratory values with linezolid exposure. Nearly all phase III efficacy trials with linezolid employed 600mg twice daily as the administration regimen; therefore the range of exposure was limited.
1.1 Absorption
Linezolid is rapidly and extensively absorbed after oral administration,[18,19,23] with Cmax usually achieved 1–2 hours after administration.[16–20] Based on area under the concentration-time curve (AUC), a marker of the overall extent of absorption, the absolute bioavailability of an oral dose is complete. The high oral bioavailability demonstrates that linezolid can be administered by either the intravenous or oral route without the need for dosage adjustment. Concentration profiles following intravenous and oral administration of single doses of 375mg (figure 2) demonstrate the equivalence of the two routes based on AUC.[18]
Linezolid plasma concentrations after administration of a 375mg dose either orally or intravenously. Values are means ± SD (n = 12 [seven males and five females]). The calculated area under the concentration-time curve to infinity for these profiles were 50 and 52 mg · h/L for intravenous and oral administration, respectively.[18]
Oral absorption (AUC) of linezolid is not affected by food; only a slight decrease in Cmax (about 18%) and a slightly later time to Cmax (about 2 hours versus about 1.5 hours) were observed. Food did not affect oral bioavailability; therefore, linezolid can be taken with or without food.[18]
1.2 Distribution
The distribution of linezolid is approximately that of total body water, as the steady-state volume of distribution averages 40–50L.[16–18,24,25]
The protein binding of linezolid is to serum albumin and is relatively low (31%), indicating that measurement of total plasma concentrations of linezolid is appropriate for calculating the pharmacokinetic parameters.[26]
Linezolid distribution and tissue penetration in selected sites are summarised in table II. The intrapulmonary pharmacokinetics of linezolid have been assessed.[27] Linezolid is present in epithelial lining fluid at concentrations about 2–6 times higher than in plasma at the corresponding time points. Linezolid was also present in alveolar cells but at a lower concentration than in plasma. In general, Cmax was observed at the 4-hour time point. Concentrations of linezolid in saliva were approximately 25% higher than in plasma, whereas concentrations in sweat were approximately 45% lower than in plasma.[16] Linezolid does not appear to be extensively distributed into red blood cells.[23]
The distribution of linezolid into skin blister fluid has been assessed. The Cmax in blister fluid occurred at 3 hours. The average AUC values for plasma and blister fluid were 140.3 and 155.3 mg · h/L, respectively. Penetration into the inflammatory fluid, determined as the individual ratio of blister fluid AUC to plasma AUC, was 104% ± 20.7%. These results indicate that linezolid has good tissue penetration and should be effective in treating tissue infections.[28]
Linezolid distribution into bone, synovial fluid and muscle was assessed following administration of 600mg twice daily. The average linezolid concentrations in bone, synovial fluid and muscle were 8.49 mg/kg, 20.1 mg/L and 18.5 mg/kg, respectively, relative to a linezolid plasma concentration of 23.0 mg/L.[29] In a single-dose evaluation, the concentrations of linezolid in plasma, bone and synovial fluid were 6.9, 2.4, and 7.7 mg/L, respectively.[30] The penetration into bone following single and multiple doses was 33% and 40.1%, respectively.[29,30]
1.3 Metabolism
Linezolid circulates mainly as parent drug in patients without severe renal impairment. Under steady-state conditions, the plasma AUC of the most abundant metabolite is equivalent to only 20–30% of the linezolid AUC, indicating that systemic exposure of patients to linezolid will exceed that of its metabolites. The metabolites do not have significant antibacterial activity relative to linezolid.
There are three main pathways in the clearance of linezolid: excretion of intact linezolid in urine, and two distinct nonrenal pathways that form the oxidative product metabolites PNU-142300 and PNU-142586, respectively (figure 3).[23] Of these two major nonrenal elimination pathways, PNU-142300 represents a relatively constant and low 9–11% of dose. In vitro studies on the possible roles of the major oxidases involved in drug metabolism (cytochrome P450 [CYP], flavin mono-oxygenase and monoamine oxidase [MAO]), showed that formation of the major metabolite, PNU-142586, is not mediated by major human isoforms of these enzymes. In vitro studies using human liver microsomes also showed that the formation of PNU-142586 is initiated by a chemical oxidation that is a nonenzymatic (noncatalytic) process. The enzymes or oxidants that contribute to PNU-142586 formation in vivo have not been elucidated.
In in vitro, animal and human studies, linezolid is not detectably metabolised by CYP,[31] and it does not induce or inhibit the activities of clinically significant human CYP isoforms (1A2, 2C9, 2C19, 2D6, 2E1 and 3A4).[31–33]
1.4 Excretion
After single or multiple intravenous doses, the total systemic clearance (CL) of linezolid was approximately 100–200 mL/min. Renal clearance (CLR) averaged 30–50 mL/min, which suggests net tubular reabsorption. Nonrenal clearance, calculated as the difference between CL and CLR, averaged 70–150 mL/min. The elimination half-life averaged 5–7 hours.[17,19,20] Studies with radiolabelled linezolid 500mg (as [14C]linezolid 100 µCi) were conducted with single and multiple doses. Mass balance measurements accounted for approximately 94% of the dose in urine and faeces. Approximately 35% of the dose was excreted in urine as the parent drug and approximately 50% was excreted as the two major metabolites (approximately 40% as PNU-142586 and 10% as PNU-142300). Approximately 10% of the dose was excreted as the two major metabolites in the faeces.[23]
2. Factors Affecting Pharmacokinetics
2.1 Age
The pharmacokinetics of linezolid in elderly subjects were assessed as part of a study designed to evaluate the effects of age and sex on the pharmacokinetics of linezolid. In that study, six elderly men aged 65–74 years (mean 70 years) and eight elderly women aged 65–75 years (mean 70 years) were compared with eight young men aged 21–38 years (mean 39 years) and seven young women aged 21–38 years (mean 30 years). The pharmacokinetics of linezolid were determined for each subject following a single 600mg oral dose. The pharmacokinetic parameters are summarised in table III.
Except for CLR, which was correlated with creatinine clearance (CLCR), there were no significant differences in pharmacokinetic parameters between the young and elderly groups. This study indicated that increased age does not alter the pharmacokinetics of linezolid and that no dosage adjustment would be necessary in elderly patients.[34]
2.2 Sex
The study described for elderly subjects[34] was also used to determine the effects of sex on the pharmacokinetics of linezolid following a single 600mg oral dose to age-matched men and women.
There was a significant difference between men and women, with mean AUC for women being approximately 64% greater than that for men (table III). This would be expected in part due to the difference in bodyweight between men and women, since each group received a fixed dose of 600mg. Based on bodyweight, women received a dose of about 9–10 mg/kg and men received a dose of about 7–8 mg/kg. There were no significant differences between men and women in the mean apparent elimination rate constant or half-life. The mean CL/F for women was 37% lower than that for men when not adjusted for bodyweight. The difference was reduced to 20% when adjusted for bodyweight. A slightly lower volume of distribution was observed in women as compared with men.
Although the mean total clearance is approximately 20% lower in women than in men, when corrected for bodyweight, the elimination rate and half-life are not sex-dependent. A dosage adjustment based on sex is not warranted because of the wide range of linezolid concentrations that are well tolerated, the similarity in half-life and expected accumulation with multiple doses, and the small difference in disposition between men and women.[34]
2.3 Hepatic Dysfunction
Linezolid has been studied in patients with hepatic impairment.[35] Eight patients with mild to moderate liver disease by Child-Pugh scores were compared with eight healthy subjects. Similar plasma linezolid concentrations were observed, and no statistically significant differences in linezolid pharmacokinetic parameters were found for patients with liver disease (table III). There was a modest increase (1.3-fold) in AUC and half-life in patients with hepatic impairment versus healthy volunteers. In patients with hepatic insufficiency, as compared with healthy volunteers, CLR of linezolid decreased by a factor of 1.3.[35] The urinary excretion of the two major metabolites fell from 14% of total dose to 5.1% and from 45% to 34% (related in part to reduced formation). These changes in renal elimination were partially offset by other factors, possibly including increased biliary and faecal elimination.
No dosage adjustment for linezolid is recommended for patients with mild to moderate hepatic disease based on linezolid pharmacokinetics and its primary mode of nonenzymatic metabolism. No pharmacokinetic data are available from patients with severe hepatic impairment.
2.4 Renal Dysfunction
Despite the high proportion of linezolid excreted via the kidney (approximately 35%), the overall clearance of linezolid is not affected by decreasing renal function.[36] A single 600mg oral dose was examined in several populations: (i) healthy volunteers with normal renal function; (ii) patients with moderately impaired renal function (CLCR 30–80 mL/min); (iii) nondialysed patients with severely impaired renal function (CLCR 10–29 mL/min); and (iv) patients with end-stage renal disease requiring haemodialysis. Linezolid plasma concentrations were similar regardless of renal function. Total clearance of linezolid did not change as a function of CLCR, but CLR decreased with decreasing renal function. CLR and CLCR were well correlated, but this had little effect on the overall clearance of linezolid, which did not decrease with reduced CLCR due to a compensatory increase in the nonrenal clearance. Therefore, no dosage adjustment for linezolid is required to maintain similar linezolid concentrations regardless of renal function.
Exposure to the two primary metabolites of linezolid (as measured by plasma AUC) after single doses in patients with severe renal insufficiency was 7–8-fold that seen in patients with normal renal function (table IV).[37] Multiple-dose administration to patients with severe renal insufficiency gave plasma concentrations of the two major metabolites that were about 10-fold higher than in subjects with normal renal function. The multiple-dose data indicate that concentrations reach a plateau during the first week of therapy and that there is no additional accumulation during four weeks of administration. The overall clinical significance of these findings has not been established, as limited safety data are currently available. Therefore, linezolid should be used with caution in patients with severe renal insufficiency. Although there was a net increase and plateau of metabolite concentrations with multiple doses in patients with severe renal impairment, the linezolid concentration profile was similar to that in patients with normal renal function.
Haemodialysis is a significant source of elimination of linezolid in the end-stage renal failure patient. Approximately one-third of the administered dose of linezolid was removed by a 3-hour haemodialysis session. The amount of drug removed will depend on the proximity of the dialysis session to the administered dose; therefore administration after dialysis is suggested.[36]
2.5 Children
The pharmacokinetic parameters of linezolid in children have been determined in three single intravenous dose studies; summary data from these studies are shown in table V.[38–41] In the initial study conducted with a low dose of 1.5 mg/kg in children between 3 months and 16 years of age, the weight-adjusted clearance value averaged about 6 mL/min/kg. This is higher than observed in adults (usually about 1–3 mL/min/kg), and the apparent elimination half-life was also shorter in children than in adults (by about half). At a dose of 10 mg/kg, up to a maximum dose of 600mg, the linezolid plasma concentrations in children were similar to those in adults at the early sampling times and for up to 1 hour postdose. However, due to the higher clearance, plasma concentrations in children at later times were lower than those in adults. Linezolid clearance was evaluated as a function of age and in general was found to be higher in younger children than in older children and adults. Children <12 years have a similar Cmax, a smaller AUC, a shorter elimination half-life and a faster clearance relative to adolescents and adults table V. These findings demonstrate the need for a higher daily dosage in these younger children, such as 10 mg/kg every 8 hours, which would result in a similar daily AUC value compared with adolescents and adults treated twice daily.
A specific study was conducted in pre- and full-term neonates and young infants (less than 12 weeks of age).[41] These data indicate that linezolid pharmacokinetics are not substantially affected by gestational age, but are a function of postnatal age (table V). Clearance normalised for bodyweight increases rather markedly during the first week of life, from values similar to those observed in adults to values in excess of those observed in older children and adults, and appears to remain relatively stable through 2–3 months of postnatal age. The mean clearance for children over a week of age of about 5 mL/min/kg is similar to the average clearance value of about 4.5 mL/min/kg observed in children between 3 and 11 months of age. As clearance rapidly increases during the first week after birth, regardless of gestational age, and since very few neonates less than a week old require an antibacterial to treat Gram-positive organisms, it is likely that newborns and young infants should also be treated with the higher daily dosage used in other children less than 12 years of age.
3. Drug Interactions
3.1 Other Antimicrobial Agents
Since linezolid has very little effect against Gram-negative organisms, a second antibacterial agent may be required in patients who have mixed Gram-positive and Gram-negative infections. Drug interaction studies were conducted for linezolid administered with aztreonam or gentamicin. No pharmacokinetic drug-drug interaction was observed when linezolid was administered with either drug.[24,25] No antagonism or synergy in antibacterial effect has been observed when linezolid is combined with aztreonam or gentamicin.[5,42]
3.2 Adrenergic and Serotonergic Agents
Linezolid is a reversible inhibitor of MAO A and B.[43,44] Interactions with classic MAO inhibitors may result in a vasopressor response (evidenced by increased blood pressure) when combined with sympathomimetic amines or tyramine in food, or may induce the signs and symptoms of serotonin syndrome (evidenced by increased body temperature, neurological or CNS changes) when taken with serotonergic agents.
The potential interaction of linezolid with tyramine was assessed by using an oral tyramine challenge study to evaluate the effect on blood pressure. When linezolid was administered at a dose of 600mg twice daily, an oral dose of at least 100mg of tyramine was necessary to raise the systolic blood pressure by more than 30mm Hg.[45] This dose of tyramine (100mg) is an order of magnitude larger than that encountered even in exceptionally tyramine-rich meals, and at this level of challenge the response was not of clinical significance.
The potential for additional adrenergic response was evaluated in two placebo-controlled double-blind studies conducted in normotensive subjects. These studies evaluated the blood pressure and heart rate effects of placebo, phenylpropanolamine or pseudoephedrine alone, linezolid alone, and the combination of multiple-dose linezolid with two doses of phenylpropanolamine 25mg or pseudoephedrine 60mg given 4 hours apart. Heart rate was not affected by any of the treatments. Blood pressure was increased with both combination treatments. Coadministration of linezolid with either pseudoephedrine or phenylpropanolamine resulted in mean increases in systolic blood pressure of the order of 30–40mm Hg, compared with 5–11mm Hg increases with linezolid alone, 14–18mm Hg with either pseudoephedrine or phenylpropanolamine alone, and 8–11mm Hg with placebo. The magnitude of blood pressure changes remained within the range of blood pressure fluctuations associated with normal daily activity.[46]
The serotonergic agent dextromethorphan was coadministered with linezolid at steady state and no evidence of the serotonin syndrome was observed. No evidence of interaction was observed when measuring body temperature, cognitive function, sedation, blood pressure and pulse.[46]
3.3 Warfarin
A study was conducted to specifically assess potential for in vivo induction of CYP2C9. Warfarin serves as a good probe for CYP2C9 metabolism, and the study with linezolid showed no significant metabolism-based interaction. However, there was a marginal statistically significant decrease (10%) in maximum International Normalized Ratio (INR), the pharmacodynamic variable in the study. Therefore, typical routine monitoring of prothrombin time would be prudent if a patient were receiving both linezolid and warfarin.[33]
4. Conclusion
The clinical pharmacokinetics and pharmacodynamics of linezolid support its recommended twice-daily administration in the treatment of Gram-positive infections. Because of full oral bioavailability and lack of significant food effect, linezolid may be given intravenously or orally, with or without food, without an adjustment in dosage. Although there is a slight nonlinearity observed in the pharmacokinetics of linezolid, the degree is not sufficient to warrant any adjustment in dosage. Linezolid metabolism is by nonenzymatic oxidation, and therefore no drug interactions based on CYP inhibition or induction are expected. Drug interactions based on MAO inhibition are limited to increases in blood pressure with coadministered adrenergic agents and are not likely to be of a significant magnitude. No changes in dosage are necessary for elderly patients, or patients with mild to moderate hepatic or renal insufficiency. Linezolid should be used with caution in patients with severe renal insufficiency due increased exposure to linezolid metabolites. Due to a higher clearance observed in children, a higher daily dosage is recommended in this patient group. The pharmacokinetic profile of linezolid and its unique mechanism of action make it a valuable agent in the treatment of infections caused by Gram-positive bacteria.
References
Borek AP, Peterson LR, Noskin GA. Activity of linezolid against medically important gram-positive bacteria from 1997–2000 [abstract]. Proceedings of the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17–20; Toronto, Ontario, Canada
Jones RN, Ballow CH, Biedenbach DJ. Multi-laboratory assessment of the linezolid spectrum of activity using the Kirby-Bauer disk diffusion method: report of the Zyvox Antimicrobial Potency Study (ZAPS) in the United States. Diagn Microbiol Infect Dis 2001; 40(1–2): 59–66
Noskin GA, Siddiqui F, Stosor V, et al. In vitro activities of linezolid against important gram-positive bacterial pathogens including vancomycin-resistant enterococci. Antimicrob Agents Chemother 1999; 43: 2059–62
von Eiff C, Peters G. Comparative in-vitro activities of moxifloxacin, trovafloxacin, quinupristin/dalfopristin and linezolid against staphylococci. J Antimicrob Chemother 1999; 43: 569–73
Zurenko GE, Yagi BH, Schaadt RD, et al. In vitro activities of U-100592 and U-100766, novel oxazolidinone antibacterial agents. Antimicrob Agents Chemother 1996; 40: 839–45
Swaney SM, Aoki H, Ganoza MC, et al. The oxazolidinone linezolid inhibits initiation of protein synthesis in bacteria. Antimicrob Agents Chemother 1998; 42: 3251–5
Kloss P, Xiong L, Shinabarger DL, et al. Resistance mutations in 23 S rRNA identify the site of action of the protein synthesis inhibitor linezolid in the ribosomal peptidyl transferase center. J Mol Biol 1999; 294(1): 93–101
Prystowsky J, Siddiqui F, Chosay J, et al. Resistance to linezolid: characterization of mutations in rRNA and comparison of their occurrences in vancomycin-resistant enterococci. Antimicrob Agents Chemother 2001; 45(7): 2154–6
Dresser LD, Rybak MJ. The pharmacologic and bacteriologic properties of oxazolidinones, a new class of synthetic antimicrobials. Pharmacotherapy 1998; 18: 456–62
Cammarata SK, Schueman LK, Timm JA, et al. Oral linezolid in the treatment of community-acquired pneumonia: a phase III trial [abstract 654]. Program and abstracts of the American Thoracic Society; 2000 May 5–10; Toronto, Ontario.
San Pedro GS, Cammarata SK, Oliphant TH, et al. Linezolid versus ceftrixone/cefpodoxime in patients hospitalised for the treatment of strepococcus pneumoniae pneumonia. Scand J Infect Dis 2002; 34: 720–8
Duvall SE, Seas C, Bruss JB, et al. Comparison of linezolid to oral clarithromycin in the treatment of uncomplicated skin infections: results from a multinational phase III trial [abstract]. Program and abstracts of the 9th International Congress on Infectious Disease; 2000 Apr 10–13; Buenos Aires, Argentina.
Stevens DL, Herr D, Lampiris H, et al. Linezolid versus vancomycin for the treatment of mehticillin-resistant staphylococcus aureus infections. Clin Infect Dis 2002; 34: 1401–9
Rubinstein E, Cammarata SL, Oliphant TH, et al. Linezolid Nosocomial Pneumonia Study Group. Linezolid (PNU-100766) versus vancomycin in the treatment of hospitalized patients with nosocomial pneumonia: a randomized, double-blind, multicenter study. Clin Infect Dis 2001; 32: 402–12
Stevens DL, Smith LG, Bruss JB, et al. Linezolid Skin and Soft Tissue Infections Study Group. Randomized comparison of linezolid (PNU-100766) versus oxacillin/dicloxacillin for treatment of complicated skin and soft tissue infections. Antimicrob Agents Chemother 2000; 44: 3408–13
Pawsey SD, Daley-Yates PT, Wajszczuk CP, et al. U-100766 safety, toleration and pharmacokinetics after oral and intravenous administration. Abstracts of European Congress of Antimicrobial Chemotherapy; 1996 May 15–17; Glasgow.
Stalker DJ, Jungbluth GL, Hopkins NK, et al. Pharmacokinetics and tolerance of single and multiple-dose oral or intravenous linezolid, an oxazolidinone antibiotic, in healthy volunteers. J Antimicrob Chemo 2003; 51(5): 1239–46
Welshman IR, Sisson TA, Jungbluth GL, et al. Linezolid absolute bioavailability and the effect of food on oral bioavailability. Biopharm Drug Dispos 2001; 22: 91–7
Welshman IR, Stalker DJ, Hopkins NK, et al. Linezolid: comparative bioavailability of single doses of 600mg tablet and oral suspension formulations. Data on file, Kalamazoo, USA: Pharmacia Corporation, 1998
Jungbluth GL, Welshman IR, Hopkins NK, et al. Linezolid: single- and multiple-dose pharmacokinetics evaluation of dose proportionality. Data on file, Kalamazoo, USA: Pharmacia Corporation, 1999
Cirincione B, Phillips L, Grasela T, et al. Influence of dose responses for linezolid efficacy using Monte Carlo simulations. Annual Meeting and Exposition of the American Association of Pharmaceutical Scientists; 2000 Oct 29–Nov 2; Indianapolis (IN)
Rayner CR, Forrest A, Meagher AK, et al. Clinical pharmacokinetics of linezolid efficacy in seriously ill patients treated in a compassionate use programme. Clin Pharmacokinet 2003; In Press
Slatter JG, Stalker DJ, Feenstra KL, et al. Pharmacokinetics, metabolism, and excretion of linezolid following an oral dose of [14C]linezolid to healthy human subjects. Drug Metab Dispos 2001; 29(8): 1136–45
Lasher S, Jungbluth G, Hopkins N. A pharmacokinetic evaluation of concomitant administration of linezolid and aztreonam. J Clin Pharmacol 1999; 39(12): 1277–82
Jungbuth GL, Lasher TA, Hopkins NK, et al. Linezolid and aztreonam: a pharmacokinetic evaluation of intravenous coadministration in healthy volunteers [abstract]. Clin Infect Dis 1997; 25(2): 487
Chiba K, Uda F, Yamazaki S, et al. U-100766: In vitro protein binding of U-100766 in plasma of rats, dogs and humans. Data on file, Kalamazoo, USA: Pharmacia Corporation, 1995
Conte JE, Golden JA, Kipps J, et al. Intrapulmonary pharmacokinetics of linezolid. Antimicrob Agents Chemother 2002 May; 46(5): 1475–80
Gee T, Ellis R, Marshall G, et al. Pharmacokinetics and tissue penetration of linezolid following multiple oral doses. Antimicrob Agents Chemother 2001; 45: 1843–6
Rana B, Murnaghan C, Butcher I, et al. Penetration of linezolid into osteo-articular tissues. Southampton, UK: The British Orthopaedic Research Society, 2001 Sep 24–25
Hopkins N, Welshman I, Jungbluth, et al. Linezolid bone levels after a single 600mg oral dose. Data on file, Kalamazoo, USA: Pharmacia Corporation, 2002
Wynalda MA, Hauer MJ, Wienkers LC. Oxidation of the novel oxazolidinone antibiotic linezolid in human liver microsomes. Drug Metab Dispos 2000; 28: 1014–7
Wienkers LC, Wynalda MA, Feenstra KL, et al. In vitro metabolism of linezolid (PNU-100766): lack of induction or inhibition of cytochrome P450 enzymes and studies on the mechanism of formation of the major human metabolite, PNU-142586. Proceedings of the 39th Interscience Conference on Antimicrobial Agents and Chemotherapy. 1999 Sep 26–29; San Francisco (CA)
Azie N, Stalker D, Jungbluth G, et al. Effect of linezolid on CYP2C9 using racemic warfarin (W) as a probe [abstract]. Clin Pharmacol Ther 2001; 69(2): 21
Lasher Sisson T, Jungbluth GL, Hopkins NK. Age and sex effects on the pharmacokinetics of linezolid. Eur J Clin Pharmacol 2002; 57: 793–7
Hendershot P, Jungbluth G, Cammarata S, et al. Pharmacokinetics of linezolid in patients with liver disease [abstract]. J Antimicrob Chemother 1999; 44 Suppl. A: 55
Brier ME, Stalker DJ, Aronoff GR, et al. Pharmacokinetics of linezolid in subjects with renal dysfunction. Antimicrob Agents Chemother 2003; 47(9): 2775–80
Zyvox® (linezolid): prescribing information. Peapack, NJ: Pharmacia Corporation, 2002 Jan. Available from URL: www.pharmacia.com/prescription/PDF_Current/Zyvox.pdf [Accessed 2003 Sep 2]
Kearns GL, Abdel-Rahman SM, Blumer JL, et al. Single dose pharmacokinetics of linezolid in infants and children. Pediatr Infect Dis J 2000; 19(12): 1178–84
Jungbluth GL. Linezolid injection: single dose pharmacokinetic assessment in pediatric patients following an intravenous infusion. Data on file, Kalamazoo, USA: Pharmacia Corporation, 2002
Jungbluth GL, Welshman IR, Hopkins NK, et al. Linezolid pharmacokinetics in adolescents. Proceedings of the Pediatric Academic Societies Annual Meeting. 2002 May 4–7; Baltimore (MD)
Jungbluth GL, Welshman IR, Hopkins NK, et al. Impact of gestational and postnatal age on linezolid disposition in neonates and young infants. Proceedings of the Pediatrie Academic Societies Annual Meeting. 2002 May 4–7; Baltimore (MD)
Sweeney MT, Baldwin KF, Zurenko GE. In vitro activity of linezolid combined with other antibacterial agents. Proceedings of the 39th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1999 Sep 26–29; San Francisco (CA)
Martin Jr JP, Herberg JT, Slatter JG, et al. Although a novel IV 364/18 microtitre plate assay demonstrates that linezolid (PNU-100766) is a weak competitive (reversible) inhibitor of human MAO-A, no clinical evidence of MAO-A inhibition in clinical trials has been observed. Proceedings of the 38th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1998 Sep 24–27; San Diego (CA)
Martin JP, Dupuis MJ, Herberg JT. The development of microtiter plate-based assays for monoamine oxidases (MAO) A and B. Data on file, Kalamazoo, USA: Pharmacia Corporation, 1998
Antal EJ, Hendershot PE, Batts DH, et al. Linezolid, a novel oxazolidinone antibiotic: assessment of monoamine oxidase inhibition using pressor response to oral tyramine. J Clin Pharmacol 2001; 41(5): 552–62
Hendershot PE, Antal EJ, Welshman IR, et al. Linezolid: pharmacokinetic and pharmacodynamic evaluation of coadministration with pseudoephedrine HCl, phenylpropanolamine HCl, and dextromethorphan HBr. J Clin Pharmacol 2001; 41(5): 563–72
Acknowledgements
We thank Cheryl J. Sweet and Dorleda Royster for their assistance in manuscript preparation. Funding was received by a grant from Pharmacia Corporation. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr Stalker and Dr Jungbluth are currently affiliated with Fujisawa Heathcare Inc., and Pfizer Global Research and Development, respectively, but at the time of submitting this manuscript both were affiliated with Pharmacia Corporation.
Rights and permissions
About this article
Cite this article
Stalker, D.J., Jungbluth, G.L. Clinical Pharmacokinetics of Linezolid, a Novel Oxazolidinone Antibacterial. Clin Pharmacokinet 42, 1129–1140 (2003). https://doi.org/10.2165/00003088-200342130-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200342130-00004