Abstract
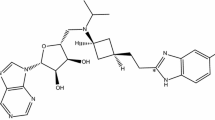
Objective: To determine the tolerability, pharmacodynamics and pharmacokinetics of single oral doses of BIA 3-202, a novel catechol-O-methyltransferase (COMT) inhibitor, in healthy male volunteers.
Methods: Single increasing oral doses of BIA 3-202 (10, 30, 50, 100, 200, 400 and 800mg) were administered under fasting conditions to seven sequential groups of nine subjects, under a double-blind, randomised, placebo-controlled design. In an additional group of eight subjects (group 8), a single dose of BIA 3-202 400mg was administered on two occasions, once under fasting conditions and once with a high-fat meal, under an open-label, two-way crossover design.
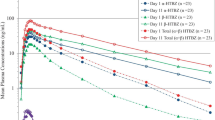
Results: BIA 3-202 was well tolerated at all doses tested. Most adverse events were mild in severity and their incidence was similar between BIA 3-202 and placebo. Maximum plasma concentrations (Cmax) of BIA 3-202 were attained at 0.522.5h (tmax) and thereafter declined with an apparent terminal half-life (t1/2) of 1.52–5h. Over the dose range of 102800mg, there was an approximately dose-proportional increase in the area under the plasma concentration-time curve (AUC) values of BIA 3-202: for a dose level increase in the ratio 3.0:1.7:2.0:2.0:2.0:2.0, AUC increased in the ratio 3.1:1.7:1.9:2.2:2.1:1.7. Plasma concentrations of the O-methylated derivative, BIA 3-270, increased markedly less than predicted from a proportional relationship: for a dose level increase in the ratio 1:80, AUC0-t increased in the ratio 1:5. In most subjects, the tmax of BIA 3-270 was attained at the last sampling time and, therefore, t1/2 could not be estimated. Urine assays showed that less than 1% of the total dose admi nistered was excreted in urine as BIA 3-202. Urine concentrations of BIA 3-270 were below the limit of quantification. In group 8, the rate and extent of systemic availability (tmax, AUC and Cmax) of BIA 3-202 and BIA 3-270 after a high-fat meal were similar to those under fasting conditions. Inhibition of COMT activity in erythrocytes reached maximum levels at 2–2.5h post dose, with sustained inhibition up to approximately 4–6 hours, returning to baseline by about 16 hours.
Conclusion: BIA 3-202 was well tolerated at single 10–800mg oral doses and presented dose-proportional kinetics. It effectively inhibited COMT activity and the presence of food did not affect its pharmacokinetics or COMT inhibitory activity. The results provide a basis for further clinical studies with BIA 3-202.









Similar content being viewed by others
References
Olanow CW, Watts RL, Koller WC. An algorithm (decision tree) for the management of Parkinson’s disease (2001): treatment guidelines. Neurology 2001; 56 Suppl. 5: S1–S88
Nutt JG, Fellman JH. Pharmacokinetics of levodopa. Clin Neuropharmacol 1984; 7: 35–49
Kurth MC, Adler CH. COMT inhibition: a new treatment strategy for Parkinson’s disease. Neurology 1998; 50: S3–S14
Bonifati V, Meco G. New, selective catechol-O-methyltransferase inhibitors as therapeutic agents in Parkinson’s disease. Pharmacol Ther 1999; 81: 1–36
Jost WH. Costs in the treatment of parkinsonism. J Neurology 2000; 247: 31–3
Kaakkola S. Clinical pharmacology, therapeutic use and potential of COMT inhibitors in Parkinson’s disease. Drugs 2000; 59: 1233–50
Lambert D, Waters CD. Comparative tolerability of the newer generation antiparkinsonian agents. Drugs Aging 2000; 16: 55–65
Factor SA, Molho ES, Feustel PJ, et al. Long-term comparative adexperience with tolcapone and entacapone in advanced Parkinson’s disease. Clin Neuropharmacol 2001; 24: 295–9
Shepherd J, Clegg A. Entacapone as an adjunctive treatment to levodopa in Parkinson’s disease. In Milne R, Stein K, editors. The Wessex Institute for Health Research & Development. Development and Evaluation Committee Report No 104. Southampton: Wessex Institute 1999: 1–50
Learmonth DA, Vieira-Coelho MA, Benes J, et al. Synthesis of Sch1-(3,4-dihydroxy-5-nitrophenyl)-2-phenyl-ethanone and derivatives as potent and long-acting peripheral inhibitors of catechol-O-methyltransferase. J Med Chem 2002; 45: 685–95
Bonifácio MJ, Vieira-Coelho MA, Soares-da-Silva P. Kinetic inhibitory profile of BIA 3-202, a novel fast tight-binding, reversible and competitive catechol-O-methyltransferase inhibitor. Eur J Pharmacol 2003; 460: 163–70
Parada A, Loureiro AI, Vieira-Coelho MA, et al. BIA 3-202, a novel catechol-O-methyltransferase inhibitor, enhances the availability of L-DOPA to the brain and reduces its O-methyl-ation. Eur J Pharmacol 2001; 420: 27–32
Parada A, Soares-da-Silva P. BIA 3-202, a novel catechol-O-methyltransferase inhibitor, reduces the peripheral O-methylation of L-DOPA and enhances its availability to the brain. Pharmacology 2003; 68: 29–37
Soares-da-Silva P, Vieira-Coelho MA, Parada A. BIA 3-202 is an effective inhibitor of erythrocyte and liver soluble catechol-O-methyltransferase and enhances the availability of L-DOPA to the brain. Pharmacol Toxicol 2003; 92: 272–8
Schultz E, Nissinen E, Kaakkola S. Determination of catechol-O-methyltransferase activity in erythrocytes by high performance liquid chromatography with electrochemical detection. Biomed Chromatogr 1989; 3: 64–7
Vieira-Coelho MA, Soares-da-Silva P. Ontogenic aspects of liver and kidney catechol-O-methyltransferase sensitivity to tolcapone. Br J Pharmacol 1996; 117: 516–20
Vieira-Coelho MA, Soares-da-Silva P. Effects of tolcaponeupon soluble and membrane-bound brain and liver catechol-O-methyltransferase. Brain Res 1999; 821: 69–78
Rosenzweig P, Miget N, Brohier S. Transaminase elevation on placebo during phase I trials: prevalence and significance. Br J Clin Pharmacol 1999; 48: 19–23
Dingemanse J, Jorga KM, Schmitt M, et al. Integrated pharmacokinetics and pharmacodynamics of the novel catechol-O-methyltransferase inhibitor tolcapone during first administration to humans. Clin Pharmacol Ther 1995; 57: 508–17
Schultz E, Nissinen E. Inhibition of rat liver and duodenum soluble catechol-O-methyltransferase by a tight-binding inhibitor OR-462. Biochem Pharmacol 1989; 38: 3953–6
Nissinen E, Linden IB, Schultz E, et al. Biochemical and pharmacological properties of a peripherally acting catechol-O-methyltransferase inhibitor entacapone. Naunyn Schmiedebergs Arch Pharmacol 1992; 346: 262–6
Borges N, Vieira-Coelho MA, Parada A, et al. Studies on the tight-binding nature of tolcapone inhibition of soluble and membrane-bound rat brain catechol-O-methyltransferase. J Pharmacol Exp Ther 1997; 282: 812–7
Bonifácio MJ, Vieira-Coelho MA, Borges N, et al. Kinetics of rat brain and liver solubilized membrane-bound catechol-O-methyltransferase. Arch Biochem Biophys 2000; 384: 361–7
Keranen T, Gordin A, Karlsson M, et al. Inhibition of soluble catechol-O-methyltransferase and single-dose pharmaco-kinetics after oral and intravenous administration of entacapone. Eur J Clin Pharmacol 1994; 46: 151–7
Dingemanse J, Jorga K, Zürcher G, et al. Pharmacokinetic-pharmacodynamic interaction between the COMT inhibitor tolcapone and single-dose levodopa. Br J Clin Pharmacol 1995; 40: 253–62
Palma PN, Bonifacio MJ, Loureiro AI, et al. Molecular modeling and metabolic studies of the interaction of catechol-O-methyltransferase and a new nitrocatechol inhibitor. Drug Metab Dispos 2003; 31: 250–8
Dingemanse J, Jorga K, Zurcher G, et al. Multiple-dose clinical pharmacology of the catechol-O-methyl-transferase inhibitor tolcapone in elderly subjects. Eur J Clin Pharmacol 1996; 50: 47–55
Acknowledgements
The study was funded by Bial (Portela & Ca SA), S. Mamede do Coronado, Portugal.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Almeida, L., Soares-da-Silva, P. Pharmacokinetics and Pharmacodynamics of BIA 3-202, a Novel COMT Inhibitor, during First Administration to Humans. Drugs R&D 4, 207–217 (2003). https://doi.org/10.2165/00126839-200304040-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00126839-200304040-00001