Abstract
Oseltamivir is a novel agent approved for the treatment and prevention of influenza infection and illnesses in adults and children. Assessment of data from the clinical trial programme, a US health insurance database study and postmarketing surveillance allowed a comprehensive review of the safety of oseltamivir in clinical use in subjects >1 year of age.
Oseltamivir has been studied over the course of a 5-year development programme in >11 000 subjects from North America, Europe and the Southern Hemisphere, including otherwise healthy adults, approximately 500 elderly/high-risk subjects, and children (>1000) aged 1–12 years. Safety evaluations included treatment-emergent adverse events, hospitalisations and deaths, as well as haematological and biochemical laboratory safety tests.
The data reveals that oseltamivir has simple, uncomplicated pharmacology and lacks potential for drug-drug interactions. Electrocardiogram parameters, including corrected QT interval, were unaffected by oseltamivir even at high doses. Postmarketing studies confirmed that transient gastrointestinal disturbance is the major adverse effect of oseltamivir and that this can be reduced by taking oseltamivir after a light snack. On treatment serious adverse events were reported in 1.3% of oseltamivir 75mg twice daily, 0.7% of oseltamivir 150mg twice daily and 1.2% of placebo recipients, respectively, in the clinical trial programme. Postmarketing, it is estimated that, to date, over 4 million oseltamivir prescriptions have been dispensed worldwide. Approximately 2300 spontaneous reports were received by the manufacturer over the three winter seasons of use. As these events are reported infrequently and from an unknown number of users, it is not possible to definitively assess causality or frequency of reported events. Most reports were of gastrointestinal and skin reactions. However, a clear association between the skin reactions and oseltamivir has not been established. A large study of insurance records, which permitted the assessment of the relative risk of medical events treated in the month following prescription of oseltamivir in general use, showed no evidence of increased risk of cardiac, neuropsychiatric or respiratory events for those receiving oseltamivir compared with those who did not.
To conclude, no important safety concerns have evolved which might limit the suitability of oseltamivir for the treatment and prevention of influenza in all patient populations.
Similar content being viewed by others
Oseltamivir is a novel oral agent approved for the treatment and prevention of influenza infection and illness in adults and children. Annual outbreaks of influenza affect high proportions of the population. During influenza seasons the incidence of clinical influenza can be up to 32% in families of infected individuals.[1] Any drug used to treat/prevent such a common disorder must be well tolerated and free from liability to cause significant safety problems when used in a wide general population.
This paper reviews the accumulated information on the safety of oseltamivir derived from the extensive clinical development programme conducted prior to approval and updates that information with postmarketing data from a US health insurance database study and postmarketing surveillance.
1. Sources of Data
An extensive clinical programme has been conducted to evaluate the pharmacology, pharmacokinetics, safety and efficacy of oseltamivir. While pharmacology and pharmacokinetic studies have been conducted mainly in healthy volunteers, studies evaluating oseltamivir in the treatment of influenza have included a wide range of populations and age groups, comprising adult and elderly populations, patients with chronic respiratory or cardiac conditions, and children aged 1–12 years.[2–12] Prophylaxis studies have included subjects aged 13 years and over and incorporate data from elderly residents of specialised nursing facilities. An overview of the development programme is shown in figure 1.[2–18]
Safety data collected during the development programme included treatment-emergent adverse events and laboratory biochemical and haematological tests. A large clinical pharmacology study investigated the potential for oseltamivir to affect electrocardiogram (ECG) parameters, most notably corrected QT (QTc) intervals.[9] Adverse event data were analysed in two phases: the ‘on-treatment’ period, i.e. those events which began during treatment or up to two days after the end of treatment; and ‘off-treatment’ events which began after the ‘on-treatment’ phase and represent the usual range of medical events experienced by individuals being followed for periods of up to 6 weeks during the winter season.
Laboratory evaluations were performed prior to the start of treatment and immediately following the last dose in all studies that formed part of the clinical programme.[3,4,6–8,10–12,14–18] Data were analysed using evaluations of group and individual changes from baseline values and shift frequency tables, assigning absolute laboratory values using the WHO recommended toxicity grading scale. This evaluation focuses upon the safety of oseltamivir observed at the dose regimens licensed for use in the treatment/prevention of influenza in comparison with placebo.
Additionally this paper presents information derived from the spontaneous reports received by the manufacturer postmarketing up to and including 30 September 2001. Between the first approval of oseltamivir for the treatment of influenza in adults in Switzerland and this date, it is estimated that approximately 4 million prescriptions have been dispensed worldwide.
Finally, safety data derived from a retrospective cohort study using data reported within 30 days following a prescription for oseltamivir for patients with an influenza-like illness enrolled in the United Healthcare Insurance System are described.[17] These data are compared with data reported in the same time period from patients with an influenza-like illness for which no oseltamivir were dispensed.
2. Data from the Clinical Programme
2.1 Clinical Pharmacology
The clinical pharmacology of oseltamivir is simple and well understood.
2.1.1 Absorption and Bioavailability
Oseltamivir is a pro-drug that is readily absorbed from the gastrointestinal tract and extensively converted by hepatic carboxylesterases to the single active metabolite, oseltamivir carboxylate (Ro64-0802). The absolute bioavailability of oseltamivir in the form of the carboxylate is approximately 75–80%.[2] Measurable plasma concentrations of carboxylate are found within 30 minutes, reach near-maximal levels in 2–3 hours post-dose, and substantially exceed (>20-fold) those of oseltamivir. Plasma concentrations of both oseltamivir and its metabolite were proportional to dose after single doses of up to 1000mg and displayed only a small degree of intra and inter-subject variability.[2] Food has minimal effects on the kinetics of oseltamivir indicating that the drug could be administered in any temporal relation to a meal.[2] Administration under conditions of altered gastric pH, such as that induced by cimetidine and antacids, did not alter the rate or extent of absorption of oseltamivir.[2]
2.1.2 Distribution
The protein binding of oseltamivir is approximately 42%, and a negligible fraction (<3%) of the carboxylate was bound to human plasma proteins at any concentration.[2] Oseltamivir and its carboxylate distribute well into the sites of influenza infection (e.g. lung, trachea, nasal mucosa and middle ear) and the concentration of carboxylate at these sites is high enough to inhibit viral replication.[19–21] The volume of distribution (Vss) of the carboxylate in humans following intravenous administration was 23–26L, which is similar to the extra-cellular volume of body water, suggesting that the active metabolite penetrates the areas of viral infection at concentrations similar to those in plasma.[2] This was subsequently confirmed in a small study in which sinus and middle ear fluid concentrations were measured.[19]
2.1.3 Metabolism
At least 75% of an oral dose of oseltamivir is converted to the carboxy metabolite by first-pass metabolism and <5% is recovered in urine as the pro-drug. In vitro studies show that neither oseltamivir nor its active metabolite interacts with human cytochrome P450 mixed-function oxidases or glucuronyl transferases.[2] Moreover, oseltamivir and the carboxylate are the only compounds found in human excreta after oral or intravenous administration of oseltamivir.[2]
2.1.4 Elimination
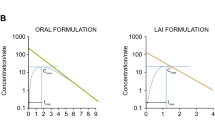
Following conversion to the carboxylate, the remaining oseltamivir and its carboxylate are eliminated exclusively by renal excretion. Plasma concentrations of orally administered oseltamivir decline rapidly with an apparent elimination half-life of 1–3 hours in most subjects. However, post-peak plasma concentrations of the active metabolite decline less rapidly with an apparent half-life of 6–10 hours, permitting twice daily administration.[2]
Renal clearance of both oseltamivir and its carboxylate exceeds the glomerular filtration rate, indicating that renal tubular secretion contributes to the elimination of the compound. This has been shown to occur via the anionic transport process.
2.1.5 Multiple Dose Pharmacokinetics
The pharmacokinetics of oseltamivir are linear and dose-proportional at doses of up to 500mg twice daily, only modest accumulation (<2-fold) of the carboxylate being noted prior to steady-state.[2] Pharmacokinetics during multiple dose administration are predictable from single dose administration and provide no indication of a temporal change in the disposition of either moiety. Steady-state plasma concentrations are achieved within 2–3 days of twice daily administration.[2] During twice daily administration of 75mg oseltamivir, plasma levels of the active metabolite remained above the inhibitory concentrations (IC50 values) of all influenza virus strains tested in vitro over the dosing interval.[2]
2.1.6 Pharmacokinetics in Special Patient Populations
Overall, there are no clinically relevant differences in the pharmacokinetics of oseltamivir between healthy volunteers and subjects infected with influenza virus.[2] In addition, there was no clinically relevant effect of sex, age or weight on the pharmacokinetics of either the prodrug or metabolite in adult patients.[2] The pharmacokinetics of oseltamivir and Ro 64-0802 in Japanese and Caucasian subjects were found to be similar indicating that the pharmacology of the drug is not ethnically sensitive.[5-13]
In elderly patients, drug exposure increases in proportion to the usual age-related decline in renal function.[2] However, as the increase in exposure is small relative to the known safety margin, no dose adjustment is necessary in this population.
As expected, in subjects with renal impairment, exposure to the active metabolite is increased as a function of decreased renal function, a marked increase in exposure being associated with severe renal impairment (creatinine clearance [CLCR] rates of <30 mL/min).[2] Therefore dose reductions are recommended for patients with severe renal impairment. Oseltamivir is not recommended in patients with end stage renal disease (CLCR <10 mL/min).
Metabolism of the prodrug to the carboxylate occurs via high capacity carboxylesterases in the liver. In vitro experiments have shown that this metabolic pathway is unlikely to be significantly affected in subjects with moderate hepatic impairment, and this has been confirmed in a kinetic study.[22] Therefore, no dose adjustments are necessary in subjects with mild to moderate hepatic impairment.
The pharmacokinetics of oseltamivir and Ro 64-0802 are similar between healthy children and children with naturally acquired influenza.[23] Young children clear the carboxylate faster than adults resulting in lower exposure to the drug for a given mg/kg dose. With advancing age, the difference in exposure between children and adults becomes less, such that the pharmacokinetic profile and exposure in children aged 13 years and over is similar to that in adults given the same dose.
While the range of exposures in children aged 1–12 years and adolescents aged 13–16 years following a 2 mg/kg dose of oseltamivir fell within the range of exposures established to be safe and effective in adults receiving either 75mg or 150mg twice daily doses, a clear trend towards higher systemic clearance following the same mg/kg dose in younger children was evident.[23] Therefore, drug administration guidelines were developed to provide exposures in children similar to those shown to be safe and effective in adults. The drug administration guideline was based on a target exposure window and a simple linear regression analysis of pharmacokinetic data collected in children and adolescents following a single 2 mg/kg dose of oseltamivir. It was expected that age- and weight-based unit drug administration would be simple to use and would reduce the potential for errors in calculating dose based on a mg/kg basis.
The predicted area under the concentration-time curve (AUC)0-∞ following 30, 45 and 60mg doses of the oral suspension (12 mg/mL) and a 75mg dose were first calculated using ideal weights, and then using the actual weights of children in whom efficacy and safety data were collected during the clinical studies. The drug administration guidelines were shown to be appropriate for children and adolescents to maintain drug exposure within the target safety/efficacy window and to allow for a convenient administration regimen.[23]
2.2 Drug Interaction Potential
Available data indicate that the potential for drug-drug interactions with oseltamivir is minimal. Plasma protein binding is low, indicating that drug-drug interactions via protein binding displacement are unlikely. In addition, oseltamivir has a high solubility over a broad pH range, which demonstrates that its absorption would not be affected by drugs which alter gastric pH. It does not interact with substrates of various isoforms of cytochrome P450, and interaction with these enzymes appears to be unlikely. The potential for drug interaction is limited to a potential for interference via carboxyesterase metabolism or by interaction within the anionic tubular pathway in the kidney.
This has been studied by a programme of targeted interaction studies using representative drugs with potential for interaction at each point.[24–27] The kinetic profile of oseltamivir is unaffected by moderate hepatic impairment, confirming the high capacity of hepatic carboxyesterases noted in vitro. No kinetic interaction was observed when oseltamivir was co-administered with aspirin (acetylsalicylic acid), an agent co-metabolised by carboxyesterases.[24] Oseltamivir carboxylate binds weakly to isolated humanised anionic tubular transporter protein and did not interact with amoxicillin.[25] Co-administration of amoxicillin had no effect on oseltamivir carboxylate kinetics, although probenecid, a highly potent inhibitor of the anionic tubular excretion pathway, increased carboxylate exposure by 2.5-fold, an increase that is not clinically significant due to the wide safety margin of oseltamivir. These data confirm the low probability of any significant drug-drug interaction at the level of tubular excretion.[25] Thus, under normal circumstances, oseltamivir can be co-administered with most drugs due to its wide safety margin and low drug-drug interaction potential.
2.3 Treatment-Emergent Adverse Events
2.3.1 Treatment Studies in Adult Populations
All studies in the pooled adult safety population evaluated a treatment duration of 5 days.[3,4,7,8,11,17] Transient gastrointestinal disturbances (nausea and vomiting) were the only adverse events consistently reported more frequently by subjects taking oseltamivir compared with placebo recipients (odds ratios [OR] of 1.58 [95% CI 1.19–2.10] for nausea and 2.64 [95% CI 1.77–3.93] for vomiting). Taking oseltamivir after a light snack significantly reduced the incidence of nausea. Increasing doses of oseltamivir resulted in a higher incidence of nausea and vomiting but increased exposure to the carboxylate — as a result of decreased renal clearance — had no effect on the incidence of these events indicating that they are most likely a result of mucosal irritation. These events were reported for the first time on either day 1 or 2 of treatment in the majority of those affected and occurred on only a single occasion in >90% of those affected. Given this profile it is not surprising that these events resulted in ≤1% of subjects withdrawing from the studies.
Gastrointestinal events with oseltamivir were less frequently reported among elderly subjects than those <65 years of age (figure 2). Indeed, the incidence of these events, particularly nausea and vomiting, in the elderly population was very similar to that with placebo. Thus, there is no evidence that gastrointestinal disturbance will interfere with concomitantly taken drugs needed for the control of chronic medical conditions in elderly populations.
In view of the known association between influenza and deaths from cardiac disorders an extensive review of cardiac safety was conducted. Preclinical studies showed no evidence that oseltamivir has potential for effects on cardiac repolarisation in humans.[9] Nevertheless, a large study investigating the potential for effects on the QTc-interval in humans was conducted.[9] Groups of 100 volunteers were randomised to receive placebo or oseltamivir, at twice-daily doses of 75, 225 or 450mg for 5 days (i.e. up to six times the dose recommended for the treatment of influenza). During this period, ECG measurements were taken repeatedly, and for each individual the data were compared with that collected throughout the day prior to drug administration. All ECGs were read by a central laboratory. There was no evidence that oseltamivir had any effect on QTc-intervals in this study. The incidence of abnormalities of T wave morphology was the same in all four treatment groups and comparable to that previously reported from healthy volunteer studies.
Overall, the incidence of cardiac disorders during the treatment studies was substantially lower in oseltamivir recipients than those receiving placebo (table I). Considering that the population studied included those with pre-existing cardiac conditions in addition to a considerable number of elderly subjects, these data support the conclusion that oseltamivir carries no potential for cardiac toxicity in humans.
2.3.2 Treatment Studies in Children
The safety of influenza treatment with oseltamivir in children aged 1–12 years has been evaluated in clinical studies involving >1000 subjects.[6,16,23] These studies evaluated a treatment duration of 5 days. Oseltamivir was generally well tolerated during these studies. Once again gastrointestinal events — notably vomiting — were the most frequently reported with an OR of 1.61 (95% CI 1.15–2.26) over placebo.[6,16,23] Vomiting was more frequently reported in children >6 years (table II) in both treatment groups. Interestingly, in the preschool age children the observed excess in the incidence of vomiting compared with placebo was somewhat lower than in older children. Once again these events were seen immediately following the start of treatment, resolved rapidly and did not result in any evidence of dehydration. Fewer than 1% of children stopped oseltamivir treatment because of these events.
Approximately half of the children aged ≥6 years were asthmatic. Oseltamivir had no adverse effect on pulmonary function in this population. Pulmonary function tests comprising forced expiratory volume in 1 second (FEV1) and peak expiratory flow rate (PEFR) were measured in all asthmatic children at baseline (on study enrolment) and day 6. In addition, PEFR was measured (always prior to bronchodilator use) in the morning of each day of the study. In the influenza-infected asthmatic children, on day 6 the median FEV1 value had increased by 10.8% in the oseltamivir group compared with 4.7% in the placebo group (p = 0.0148). Among the non-infected population there was no overall effect on PEFR or FEV1, the median change in peak flow from baseline was 5.6% in the placebo group compared with 5.9% for oseltamivir.
The proportion of subjects reporting an asthma exacerbation at any point post-initiation of the study was slightly lower in the oseltamivir treatment arm (18%) compared with placebo (20%). Thus, there is no evidence to suggest that treatment with oseltamivir exerts any adverse effect on respiratory function as defined by PEFR or FEV1, or reported asthma exacerbation in children with asthma.
Overall, there was no increased risk of any adverse event with oseltamivir treatment in elderly patients or children, including those patients with pre-existing cardiac or pulmonary diseases.
2.4 Safety in the Prevention of Influenza
Prolonged administration of oseltamivir 75mg once daily for up to 6 weeks for prevention of influenza in all studies was well tolerated in adults (table III).[14,15] Gastrointestinal events were less frequent in these otherwise healthy individuals than in subjects with acute influenza illness. The types of adverse events reported in elderly subjects were similar, although the overall frequency of adverse event reporting was lower in studies in the elderly than in those in younger adults receiving oseltamivir for 6 weeks (table IV).
Amantadine, and to a lesser extent rimantadine, are known to have adverse CNS effects, including both neurological and psychiatric disorders.[28] In contrast, there have been no reports of seizures in oseltamivir prophylaxis studies even though these studies included ten subjects with concurrent epilepsy or convulsions. Table V compares the reported incidence of CNS events in elderly subjects receiving amantadine prophylaxis (derived from literature sources) with the reported event frequency in elderly subjects receiving oseltamivir prophylaxis. These data suggest that oseltamivir can be expected to be better tolerated than amantadine in this population.[29]
2.5 Hospitalisations
The incidence of serious adverse events requiring hospitalisation was low in the treatment studies in adults.[31] Only two different events (pneumonia n = 4, bronchitis n = 3) were recorded in more than a single subject receiving oseltamivir; both are well-recognised sequelae of influenza infection. A case of pseudomembranous colitis and abdominal pain in one subject receiving oseltamivir 75mg twice daily was considered possibly related to treatment, with all other events considered unrelated to treatment. In this case, the subject had undergone a laparoscopic appendectomy following which a broad spectrum penicillin sulfabactam medication was administered. This event is a well described complication of broad spectrum antibiotic treatment and thus the balance of probability is that the event was related to the receipt of this drug rather than to oseltamivir.
2.6 Deaths
There were five deaths during the clinical programme. One death occurred in the treatment study in adults with either chronic respiratory disease or chronic cardiac disease.[9] The individual was a 38-year-old female who received placebo and who died of acute pneumonitis with acute respiratory distress syndrome. This subject did not have influenza. The investigator considered the event and her death as unrelated to study treatment. No deaths were reported during the studies in children.
Four of the subjects included in the prophylaxis studies died.[15] Two of these received placebo and two received oseltamivir; all four were elderly residents of skilled nursing facilities. In each case, the death, and the events immediately leading up to it, occurred after the end of study medication. The causes of death were malignant disease (placebo n = 1; oseltamivir n = 1), myocardial infarction (placebo n = 1) and intestinal perforation (oseltamivir n = 1). None of the deaths was considered by the investigator to be related to study medication.[9]
2.7 Clinical Laboratory Data and Vital Signs
There were no clinically relevant changes from baseline in any of the standard haematological or biochemical tests performed. Similarly, there was no difference between groups in the numbers of individuals who exhibited shifts in the WHO grading for individual laboratory parameters.
Throughout the clinical treatment studies, no impact of oseltamivir was noted with regard to any vital sign. There was no evidence to suggest that treatment with oseltamivir exerts any adverse effect on respiratory function in children with asthma. A slightly smaller proportion of children in the oseltamivir group experienced asthma exacerbation when compared with placebo.
3. Postmarketing Surveillance
Since oseltamivir was first marketed during the winter 1999/2000 influenza season, over 4 million prescriptions have been issued worldwide.
To date, approximately 2300 spontaneous events on oseltamivir have been reported to Roche from various sources around the globe. The most frequently reported events were for disorders of the gastrointestinal, respiratory, special senses and skin systems. The events occurring in the first three systems were either related to influenza (e.g. nausea, vomiting, bronchitis, coughing, pneumonia, loss of taste) or already associated with oseltamivir (e.g. nausea and vomiting). For skin disorders (the majority of which were reported by subjects in Japan), the reports were primarily due to dermatitis, rash urticaria and eczema. Approximately 15% of reported cases were considered serious but further review of the information provided indicated that, in at least half of the cases, patients had also taken other medications which are known to be associated with hypersensitivity reactions.
Following the licensing of oseltamivir in Japan, a number of reports of liver dysfunction have been received. In the vast majority of instances, these events were associated with bacterial sepsis and/or evidence of viral hepatitis. However, based on the reported information no alternative explanation could be identified. The data sheet has been amended to include the potential for rare instances of liver dysfunction in oseltamivir recipients. As these events were reported from a population of uncertain size and information enabling an assessment of causality is limited, the relationship between these events and receipt of oseltamivir is not established. By and large, however, the type and frequency of reports received postmarketing is similar to those observed during the clinical development period, and further supports the excellent tolerability of oseltamivir in general use.
In January 2000, the US FDA issued a short advisory note concerning misdiagnosis of acute bacterial sepsis and several deaths among patients treated with both oseltamivir and zanamivir. The purpose of the release was to remind the medical profession of the duty of care to examine patients with acute fever and to prescribe an antibiotic if bacterial infection was suspected. Additional warnings were added to the zanamivir label concerning risk of bronchospasm and deaths related to respiratory failure, but these events were not observed with oseltamivir.
4. Health Outcomes in Patients Receiving Oseltamivir
A study was conducted to evaluate the health outcomes in subjects included in the United Healthcare research database, a managed care organisation in the US that provides healthcare to several million patients.[17] The primary objective of this study was to assess the risk of cardiac, neuropsychiatric and respiratory endpoints among patients diagnosed with influenza and to compare the risks with those patients who received oseltamivir for the treatment of influenza between December 1 1999 and March 31 2000. Subjects who had registered with the plan for 91 days prior to December 1 1999 and who were dispensed oseltamivir and had an international classification of diseases (ICD)-9 code of influenza (n = 3304) or who had a doctor visit with an ICD-9 code of influenza within the same timeframe but who were not prescribed oseltamivir (n = 28 948), were included in the analysis. The follow-up period was 30 days after the diagnosis of influenza in both groups of patients.
All events were evaluated in patients with and without risk factors for these for these cardiac, neuropsychiatric and respiratory conditions prior to the influenza diagnosis or receipt of oseltamivir.
Among the 32 252 subjects diagnosed with influenza, subjects who received oseltamivir were slightly older (mean age 39 years) than those who did not receive oseltamivir (mean age 30 years). With this exception the groups were well balanced for important demographic features, including the proportion of subjects with baseline risk factors of chronic respiratory, cardiac or neuropsychiatric conditions (table VI).
Baseline characteristics of subjects in the United Healthcare research database with an ICD-9 code of influenza receiving oseltamivir (75mg bid for 5 days) compared with those not receiving this treatment between 1st Dec 1999 to 31st Mar 2000[17]
Table VII displays the adjusted relative risks of the 30-day incidence of cardiac, neuropsychiatric and respiratory events in subjects with/without a history of risk factors, respectively, adjusted for age and other influenza medications. The data show that even in subjects with risk factors for the development of these conditions there was no evidence of increased risk of cardiac, neuropsychiatric or respiratory events for those receiving oseltamivir compared with those who did not. These data support the conclusion from the clinical development programme that oseltamivir is unlikely to destabilise pre-existing cardiac, neurological or psychiatric, or respiratory conditions.
Relative risks (with 95% CI) for development of a cardiac, neuropsychiatric or respiratory event within 30 days of an influenza-like illness in patients treated with oseltamivir with/without risk factors for these conditions[17]
5. Discussion
Until recently, the antiviral agents available for treatment and prevention of influenza were either ineffective against influenza B or were difficult to use and poorly tolerated by vulnerable populations.[28–30] The older M2 ion channel inhibitor amantadine, when given at doses greater than 100 mg/day is associated with dose-dependent CNS adverse reactions, especially in renally impaired subjects and in the elderly and so requires careful dose titration.[32] Rimantadine, another of the M2 inhibitors, is generally believed to have a better safety and tolerability profile than amantadine, although caution is also required when it is administered to subjects with epilepsy, and dose adjustment is needed in the renally impaired and the elderly.[32] Of further concern is that treatment of influenza illness with either amantadine or rimantadine is associated with the emergence of a high incidence (up to 30%) of resistant viruses with infectivity and pathogenicity that is equivalent to wild type.[32] This has led some to question the wisdom of using the amantadinamines for concurrent treatment of ill subjects and prophylaxis of close contacts. Because of the limitations of these compounds, a new class of drugs which inhibit the influenza virus neuraminidase have been developed. The first of these, zanamivir, must be given by inhaler, a delivery method which may not be suitable for all patients, especially children and the frail elderly. Oseltamivir, the second of the neuraminidase inhibitors, has been developed to supplement current management options. A medical alert regarding bronchospasm was sent out in the first year of sale of zanamivir, but no further cautions have been issued and its label carries appropriate warnings. The use of oseltamivir does not appear to be associated with the same rate of bronchospasm.
The pharmacological profile of oseltamivir in humans is well understood and predictable.[2] Available data indicate that the potential for drug interactions is minimal.[24,25,27] Oseltamivir is metabolised by high capacity hepatic esterases to the active metabolite oseltamivir carboxylate, which is not metabolised further. The pro-drug is primarily eliminated via renal excretion following catabolism to the active moiety.[2] Exposure to the active moiety is directly proportional to renal clearance. However, dose adjustment is recommended only when there is severe renal impairment (i.e. CLCR <30 mL/min). Thus, there is no requirement for dose adjustment for the majority of recipients, even those with age-related decreases in renal clearance.[2,22]
Oseltamivir was well tolerated in clinical trials.[3,4,6–9,14–16] Serious adverse events were reported with an equal, and low, frequency on both active drug and placebo. Upper gastrointestinal events were reported most frequently by subjects taking active drug. The excess reporting rate of these events was between 15% (1 : 6 subjects treated) and 19% (1 : 5 of the subjects treated) compared with placebo at the 75mg twice daily dosage level. In affected subjects, these events were generally of mild or moderate intensity and were short-lived. More importantly, there was no evidence for dehydration or electrolyte imbalance in subjects experiencing episodes of vomiting. In addition, postmarketing data in the form of spontaneous reports and epidemiology studies, did not reveal any major new signals which would raise any safety concerns.[17]
The safety profile observed in children <13 years of age was very similar to that previously recorded in adults and elderly subjects and no additional safety issues have been identified.[6,12,16] The safety profile in children with chronic asthma was similar to that seen in the otherwise healthy child. There was no evidence that oseltamivir exacerbates bronchoconstriction in asthmatic subjects. In contrast, there was evidence of faster return to normal peak flow rates in oseltamivir-treated children.[12]
Oseltamivir was well tolerated when used for the prevention of influenza, with no risks related to safety or toxicity identified, even in the elderly.[14,15,18] Adverse effects were limited to transient gastrointestinal disturbances and headache. Thus, the safety profile of oseltamivir is appropriate for a drug that is to be used prophylactically. Satisfactory tolerability has been established in a broad spectrum of the population, including elderly residents of skilled-nursing facilities who had significant comorbidity and were taking multiple concomitant medications. The overall low incidence of adverse CNS effects reported in elderly subjects receiving up to 6 weeks of once daily administration of oseltamivir is reassuring, and in contrast with the profile reported following amantadine prophylaxis.
6. Conclusions
The clinical safety of oseltamivir has been extensively investigated in a large clinical development programme and postmarketing surveillance. No important safety concerns have evolved which limit the suitability of oseltamivir for the treatment of influenza in all patient populations. Similarly, oseltamivir is well tolerated when prescribed to otherwise healthy adults/adolescents and the elderly for the chemoprophylaxis of influenza. Oseltamivir is an important addition to available therapies for the management of influenza within communities.
References
Nicholson KG, Webster RG, Hay AJ, editors. Textbook of influenza. Oxford: Blackwell Science, 1998
He G, Massarella J, Ward P. Clinical pharmacokinetics of the prodrug oseltamivir and its active metabolite Ro 64-0802. Clin Pharmacokinet 1999; 37: 471–84
Treanor JJ, Hayden FG, Vrooman PS, et al. Efficacy and safety of the oral neuraminidase inhibitor oseltamivir in treating acute influenza: a randomized controlled trial. US Oral Neuraminidase Study Group. JAMA 2000; 283: 1016–24
Nicholson KG, Aoki FY, Osterhaus ADME, et al. Efficacy and safety of oseltamivir in treatment of acute influenza: a randomised controlled trial. Lancet 2000; 355: 1845–50. [Erratum correction, Lancet 2000; 356: 1856]
Kashiwagi S, Kudoh S, Watanabe A, et al. Clinical efficacy and safety of the selective oral neuraminidase inhibitor oseltamivir in treating acute influenza: placebo-controlled double-blind multicenter phase III trial. Kansenshogaku Zasshi 2000; 74: 1044–61
Whitley RJ, Hayden FG, Reisinger KS, et al. Oral oseltamivir treatment of influenza in children. Pediatr Infect Dis J 2001; 20: 127–33
Martin C, Mahoney P, Ward P. Oral oseltamivir reduces febrile illness in patients considered at high risk of influenza complications [abstract W22-7]. World Congress Options for the Control of Influenza IV; 2000 Sep 23-28; Hersonissos, Crete
Zaug M, Mahoney P, Ward P. Effective treatment of influenza with oral oseltamivir in a vaccinated population of high risk patients [abstract W23-8]. Options for the Control of Influenza IV; 2000 Sep 23-28; Hersonissos, Crete
F. Hoffmann-La Roche, 2002 (Data on file)
Whitley R, Dutkowski R, Ipe D, et al. Safety and acceptability of oseltamivir liquid formulation in the treatment of influenza in children aged 1 to 12 years [abstract]. International Congress Infectious Diseases 2000 Apr 10-13, Buenos Aires, Argentina
Martin C, Mahoney P, Ward P. Oral oseltamivir reduces febrile illness and is safe in patients with chronic cardiac and/or respiratory disease [abstract]. European Respiratory Society (ERS), 2000 Aug 30-Sep 3, Florence, Italy
Whitley RJ, Reisinger KS, Hayden FG, et al. Oral oseltamivir is effective and safe in the treatment of influenza virus infections in children [abstract]. European Respiratory Society (ERS), 2000 Aug 30-Sep 3, Florence, Italy
Kashiwagi S, Kudoh S, Watanabe A, et al. Efficacy and safety of the selective oral neuraminidase inhibitor oseltamivir for prohylaxis against influenza: placebo-controlled double-blind multicenter phase III trial. Kansenshogaku Zasshi 2000; 74: 1062–76
Welliver R, Monto AS, Carewicz O, et al. Effectiveness of oseltamivir in preventing influenza in household contacts. JAMA 2001; 285: 748–54
Peters P, Gravenstein S, Norwood P, et al. Long-term use of oseltamivir for the prophylaxis of influenza in a vaccinated frail older population. J Am Geriatr Soc 2001; 49: 1025–31
Waskett N, Mahoney P, Gilbride J, et al. Safety of oseltamivir in clinical use in children and adults [abstract]. Durban, South Africa: WONCA, 2001 May 13-17
Thakrar B, Dutkowski R, Froelich E, et al. Oseltamivir is well tolerated by all patient groups [abstract]. ECC, 2002 May 5-8, Paris, France
Hayden FG, Atmar RL, Schilling M, et al. Use of the selective oral neuraminidase inhibitor oseltamivir to prevent influenza. N Engl J Med 1999; 341: 1336–43
Kurowski M, Barrett J, Waalberg E, et al. Oral oseltamivir rapidly delivers active drug levels to middle ear and sinuses in humans [abstract 509]. 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17-20; Toronto (ON)
Wiltshire HR, Muir J, Lambkin R, et al. Distribution pattern of GS-4071, a novel influenza neuraminidase inhibitor, following oral administration of its prodrug GS4104 in the ferret model [abstract]. ESCV 1998 Aug 30-Sep 2, Hamburg, Germany
Kurowski M, Oo C, Wiltshire H, et al. Oseltamivir distributes to influenza virus replication sites in the upper respiratory tract. Clin Pharmacol Ther. In press
Oo C, Snell P, Lieu B, et al. No dose adjustment of an anti-influenza prodrug oseltamivir is required in patients with hepatic impairment. 4th European Congress of Chemotherapy and Infection; 2002 May 4-7; Paris, France
Oo C, Barrett J, Hill G, et al. Pharmacokinetics and dosage recommendations for an oseltamivir oral suspension for the treatment of influenza in children. Paediatr Drugs 2001; 3: 229–36
Oo C, Barrett J, Dorr A, et al. Lack of pharmacokinetic interaction between the oral anti-influenza prodrug oseltamivir and aspirin. Antimicrob Agents Chemother 2002; 46: 1993–5
Hill G, Cilhar T, Oo C, et al. The anti-influenza drug oseltamivir exhibits low potential to induce pharmacokinetic drug interactions via renal secretion: correlation of in vivo and in vitro studies. Drug Metab Dispos 2002; 30: 13–9
He G, Massarella J, Ward P. Clinical pharmacokinetics of the prodrug oseltamivir and its active metabolite Ro 64-0802. Clin Pharmacokinet 1999; 37: 471–84
Snell P, Oo C, Dorr A, et al. Lack of pharmacokinetic interaction between the oral anti-influenza drug oseltamivir and antacids. Br J Clin Pharmacol 2002; 54: 372–7
Hayden FG, Gwaltney Jr JM, Van de Castle RL, et al. Comparative toxicity of amantadine hydrochloride and rimantadine hydrochloride in healthy adults. Antimicrob Agents Chemother 1981; 19: 226–33
Keyser LA, Karl M, Nafziger AN, et al. Comparison of central nervous system adverse effects of amantadine and rimantadine used as sequential prophylaxis of influenza A in elderly nursing home patients. Arch Intern Med 2000; 160: 1485–8
Stange KC, Little DW, Blatnik B. Adverse reactions to amantadine prophylaxis of influenza in a retirement home. J Am Geriatr Soc 1991; 33: 700–5
Kaiser L, Wat C, Mills T, et al. Impact of oseltamivir treatment on influenza-related lower respiratory tract complications and hospitalizations. Arch Intern Med 2003; 163(14): 1667–72
Kucers A, Crowe SM, Grayson ML, et al., editors. The use of antibiotics: a clinical review of antibacterial, antifungal and antiviral drugs. Oxford: Butterworth-Heinmann, 1997: 1834–54
Acknowledgements
This study was funded by Hoffman La-Roche Ltd.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dutkowski, R., Thakrar, B., Froehlich, E. et al. Safety and Pharmacology of Oseltamivir in Clinical Use. Drug-Safety 26, 787–801 (2003). https://doi.org/10.2165/00002018-200326110-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200326110-00004