Summary
Labetalol was the first of a new class of antihypertensive drugs with both α- and β-adrenoceptor blocking properties present in the same molecule. Its efficacy has been confirmed by double-blind studies in the treatment of all grades of hypertension and in angina pectoris. The drug’s major dose-related side effect is postural hypotension.
The clinical formulation of labetalol consists of equal proportions of 4 optical isomers. One of these (the RR isomer) is probably responsible for the drug’s β-adrenoceptor blockade and another (the SR isomer) produces most of the α-blockade. Most of the presently available pharmacokinetic information concerning labetalol is from studies utilising a fluori-metric assay but this has recently been superceded by more specific high-pressure liquid Chromatographic (HPLC) procedures.
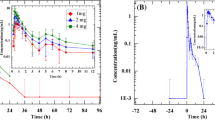
Labetalol is absorbed rapidly after oral administration with peak plasma concentrations generally being achieved within 2 hours. The bioavailability varies from 10% to over 80% in different subjects. Average bioavailability has been reported to correlate with age, with values of approximately 30% in the 30- to 40-year age group and approximately 65% at 80 years. There is also evidence that the bioavailability increases moderately when the drug is taken with food. About 50% of the drug is bound to protein in the plasma.
The apparent volume of distribution at equilibrium varies from approximately 200 to over 800L, suggesting that concentration of labetalol occurs in extravascular sites. Radiochemical analysis in animals has shown high levels of accumulation in the lung, liver and kidney with little present in brain tissue. This is in keeping with the relatively low lipid solubility of labetalol.
The half-life of labetalol in plasma is 3 to 3.5 hours. The drug is eliminated mainly by hepatic metabolism with the production of several biologically inactive glucuronides which in turn are excreted in the urine and bile. Approximately 85% of labetalol in the blood is removed during a single passage through the liver; thus, like Propranolol, iabetalol’s clearance is probably flow dependent (i.e. it is sensitive to alterations in hepatic blood flow). Small doses of the drug (i.e. 300mg daily) have been shown to reduce antipyrine clearance by approximately 15%, and further studies are necessary to determine whether high doses produce a greater, possibly clinically significant, inhibition of mixed-function oxidase activity.
After both single doses and during long term treatment the plasma concentration-time profile of labetalol shows marked variation between different individuals. A broad relationship exists between the plasma concentration and the fall in blood pressure, particularly in the upright position. However, individual sensitivity to the drug’s hypotensive action also plays a major role in determining the response.
There is only limited information available concerning the handling of labetalol in pregnancy and in disease states. In newborn infants, plasma labetalol concentrations are 30 to 50% of those of the mother and concentrations in breast milk have been reported to be 22 to 45% of the maternal plasma concentration. In chronic liver disease, bioavailability of the drug is reported to be doubled and plasma concentrations are substantially higher than in normal controls. In chronic renal disease the pharmacokinetic handling is reported to be virtually unaltered.
Similar content being viewed by others
References
Bailey, R.R.: Labetalol in the treatment of patients with hypertension and renal function impairment. British Journal of Clinical Pharmacology 8 (Suppl. 2): 135S–140S (1979).
Barnett, A.J.; Kalowski, S. and Guest, C.: Labetalol compared with pindolol plus hydrallazine in the treatment of hypertension. Medical Journal of Australia 1: 105–109 (1978).
Brittain, R.T.; Drew, G.M. and Levy, G.P.: The α- and β-adrenoceptor blocking potencies of labetalol and its individual stereoisomers in anaesthetized dogs and in isolated tissues. British Journal of Pharmacology 77: 105–114 (1982).
Blakeley, A.G.H. and Summers, R.J.: The effects of labetalol (AH5158) on adrenergic transmission in the cat spleen. British Journal of Pharmacology 59: 643–660 (1977).
Brown, J.J.; Lever, A.F.; Cumming, A.M.M. and Robertson, J.I.S.: Labetalol in hypertension (correspondence). Lancet 1: 1147 (1977).
Coevoet, B.; Leuliet, P.; Comoy, E.; Makdassi, R.; Fiovet, P.; De Fremont, J.F.; Gheerbrant, J.D.; Boulanger, J.C. and Fournier, A.: Second Congress of the International Society for the Study of Hypertension in Pregnancy, Cairo (1980).
Daneshmend, T.K. and Roberts, C.J.C.: The short term effects of Propranolol, atenolol and labetalol on antipyrine kinetics. British Journal of Clinical Pharmacology 13: 817–820 (1982a).
Daneshmend, T.K.; Homeida, M. and Roberts, C.J.C.: The effect of hepatosplenic Schistosomiasis on the pharmacokinetics of metronidazole and labetalol (abstract). British Journal of Clinical Pharmacology 14: 152P–153P (1982).
Dargie, H.J.; Dollery, C.T. and Daniel, J.: Labetalol in resistant hypertension. British Journal of Clinical Pharmacology 3 (Suppl. 3): 751–755 (1976).
Deacon, C.S.; Lennard, M.S.; Bax, N.D.S.; Woods, H.F. and Tucker, G.T.: Inhibition of oxidative drug metabolism by beta-adrenoceptor antagonists is related to lipid solubility. British Journal of Clinical Pharmacology 12: 429–431 (1981).
Dollery, C.T.: Closing remarks: Current status of labetalol. British Journal of Clinical Pharmacology 3 (Suppl. 3): 823–824 (1976).
Dusci, L.J. and Hackett, L.P.: Determination of labetalol in human plasma by high-performance liquid chromatography. Journal of Chromatography 175: 208–210 (1979).
Edwards, R.C. and Raftery, E.B.: Haemodynamic effects of long term oral labetalol. British Journal of Clinical Pharmacology 3 (Suppl. 3): 733–736 (1976).
Epstein, S.E.; Robinson, B.F.; Kahler, R.L. and Braunwald, E.: Effects of β-adrenoceptor blockade on the cardiac response to maximal and submaximal exercise in man. Journal of Clinical Investigation 44: 1745–1753 (1965).
Farmer, J.B.; Kennedy, I.; Levy, G.P. and Marshall, R.J.: Pharmacology of AH 5158; a drug which blocks both α- and β-adrenoceptors. British Journal of Pharmacology 45: 660 (1972).
George, C.F.: Drug kinetics and hepatic blood flow. Clinical Pharmacokinetics 4: 433–438 (1979).
Ghose, R.R.: Acute management of severe hypertension with oral labetalol. British Journal of Clinical Pharmacology 8: 189S–193S (1979).
Gold, E.H.; Chang, W.; Cohen, M.; Baum, T.; Ehrreich, S.; Johnson, G.; Prioli, N. and Sybertz, E.: Synthesis and comparison of some cardiovascular properties of the stereoisomers of labetalol. Journal of Medicinal Chemistry 25: 1363–1370 (1982).
Homeida, M.; Jackson, L. and Roberts, C.J.C.: Decreased firstpass metabolism of labetalol in chronic liver disease. British Medical Journal 2: 1048–1050 (1978).
Jarrott, B.; Louis, W.J. and Summers, R.J.: [3H]Guanfacine: A radioligand that selectively labels high affinityn α2-adrenoceptor sites in homogenates of rat brain. British Journal of Pharmacology 75: 401–408 (1982).
Joekes, A.M. and Thompson, F.D.: Acute haemodynamic effects of labetalol and its subsequent use as an oral hypotensive agent. Brit. J. Clin. Pharmacol. 3 (Suppl. 3): 789–794 (1976).
Jones, S.E.F.: Coarctation in children. Controlled hypotension using labetalol and halothane. Anaesthesia 34: 1052–1055 (1979).
Jureidini, K.F.; Oral labetalol in a child with phaeochromocytoma and five children with renal hypertension. Abstracts, Australasian Society of Nephrology Adelaide, 12–14 March (1980).
Kane, J.; Gregg, I. and Richards, D.A.: A double-blind trial of labetalol. British Journal of Clinical Pharmacology 3 (Suppl. 3): 737–741 (1976).
Kanto, J.; Allonen, H.; Kleimola, T. and Mantyla, R.: Pharmacokinetics of labetalol in healthy volunteers. International Journal of Clinical Pharmacology, Therapy and Toxicology 19 (No. 1): 41–44 (1981).
Kanto, J.; Allonen, H.J.; Lehtonen, A.; Mantyla, R. and Pakkanen, A.: Clinical and pharmacokinetic studies on the alpha- and beta-blocking drug labetalol. Therapeutic Drug Monitoring 2: 145–152 (1980).
Kelly, J.G.; McGarry, K.; O’Malley, K. and O’Brien, E.T.: Bio-availability of labetalol increases with age. British Journal of Clinical Pharmacology 14: 304–305 (1982).
Koch, G.: Haemodynamic effects of combined α- and β-adreno-ceptor blockade after intravenous labetalol in hypertensive patients at rest and during exercise. British Journal of Clinical Pharmacology 3 (Suppl. 3): 725–728 (1976).
Lamming, G.D.; Pipkin, F.B. and Symonds, E.M.: Comparison of the alpha and beta blocking drug, labetalol, and methyl dopa in the treatment of moderate and severe pregnancy-induced hypertension. Clinical and Experimental Hypertension 2: 865–895 (1980).
Leitz, F.; Bariletto, S.; Gural, R.; Jaworsky, L.; Patrick, J. and Symchowicz, S.: Secretion of labetalol in breast milk of lactating women. Federation Proceedings 42: 378 (1983).
Louis, W.J.; Brignell, M.J.; McNeil, J.J.; Christophidis, N. and Vajda, F.J.E.: Labetalol in hypertension (correspondence). Lancet 1: 452–453 (1978a).
Louis, W.J.; Christophidis, N.; Brignell, M.; Bijayasekaran, V.; McNeil, J.J. and Vajda, F.J.E.: Labetalol: Bioavailability, drug plasma levels, plasma renin and catecholamines in acute and chronic treatment of resistant hypertension. Australian and New Zealand Journal of Medicine 8: 602–609 (1978b).
Lund-Johansen, P. and Bakke, O.M.: Haemodynamic effects and plasma concentrations of labetalol during long-term treatment of essential hypertension. British Journal of Clinical Pharmacology 7: 169–174 (1979).
Mantyla, R.; Allonen, H.; Kanto, J.; Kleimola, T. and Sellman, R.: Effect of food on the bioavailability of labetalol. British Journal of Clinical Pharmacology 9: 435 (1980).
Maronde, R.F.; Robinson, D.; Vlachakis, N.D.; Barr, J.W.; Chung, M.; Zampaglione, N. and Medakovie, M.: Study of single and multiple dose pharmacokinetic/pharmacodynamic modelling of the antihypertensive effects of labetalol. American Journal of Medicine 75: 40–46 (1983).
Martin, L.E.; Hopkins, R. and Bland, R.: Metabolism of labetalol by animals and man. British Journal of Clinical Pharmacology 3 (Suppl. 3): 695–710 (1976).
McLean, A.J.; McNamara, P.J.; Du Souich, P.; Gibaldi, M. and Lalka, D.: Foods, splanchnic blood flow and bioavailability of drugs subject to first pass metabolism. Clinical Pharmacology and Therapeutics 24: 5–10 (1978).
McNeil, J.J.: Ph.D. Thesis, University of Melbourne (1981).
McNeil, J.J.; Anderson, A.E. and Louis, W.J.: Pharmacokinetics and pharmacodynamic studies of labetalol in hypertensive subjects. British Journal of Clinical Pharmacology 8: 157S–161S (1979).
McNeil, J.J.; Anderson, A.E. and Louis, W.J.: An analysis of the blood pressure response to labetalol in hypertensive patients. Clinical Sciences 61: 449S–452S (1981).
McNeil, J.J.; Anderson, A.E.; Louis, W.J. and Raymond, K.: Labetalol steady-state pharmacokinetics in hypertensive patients. British Journal of Clinical Pharmacology 13 (Suppl. 1): 75S–80S (1982).
McNeil, J.J. and Louis, W.J.: A double-blind crossover comparison of pindolol, metoprolol, atenolol and labetalol in mild to moderate hypertension. British Journal of Clinical Pharmacology 8: 163S–166S (1979).
Mehta, J. and Cohn, J.N.: Haemodynamic effects of labetalol, an alpha and beta adrenergic blocking agent in hypertensive subjects. Circulation 55: 370–375 (1977).
Michael, C.A.: Use of labetalol in the treatment of severe hypertension during pregnancy. British Journal of Clinical Pharmacology 8 (Suppl. 2): 211S–215S (1979).
Odendaal, H.: Use of labetalol hydrochloride in obstetrics. Medical Proceedings 25 (1): 63 (1979).
Ohnhaus, E.E.: Methods of the assessment of the effect of drugs on liver blood flow in man; in Shanks (Ed.) Methods in Clinical Pharmacology, Vol. 1, Cardiovascular System, pp. 79–85 (MacMillan, London 1980).
Poynter, D.; Martin, L.E.; Harrison, C. and Cook, J.: Affinity of labetalol for ocular melanin. British Journal of Clinical Pharmacology 3 (Suppl. 4): 711–720 (1976).
Rand, M.J.; McCulloch, M.W. and Story, D.F.: Prejunctional modulation of noradrenergic transmission by noradrenaline, dopamine and acetylcholine; in Davies and Reid (Eds) Central Action of Drugs in Blood Pressure Regulation p. 94 (Pittman Medical, London 1975).
Richards, D.A.: Pharmacological effects of labetalol in man. Brit. J. Clin. Pharmacol. 3 (Suppl. 3): 721–724 (1976).
Richards, D.A.; Prichard, B.N.C.; Boakes, A.J.; Tuckman, J. and Knight, E.J.: Pharmacological basis for antihypertensive effects of intravenous labetalol. British Heart Journal 39: 99–106 (1977).
Rosei, E.A.; Trust, P.M.; Brown, J.J.; Lever, A.F. and Robertson, J.I.S.: Intravenous labetalol in severe hypertension. Lancet 2: 1093–1094 (1975).
Rubin, P.C.; Butters, L.; Kelman, A.W.; Fitzsimmons, C. and Reid, J.L.: Labetolol disposition and concentration-effect relationships during pregnancy. British Journal of Clinical Pharmacology 15: 465–470 (1983).
Sanders, G.L.; Routledge, P.A.; Ward, A.; Davies, D.M. and Rawlins, M.D.: Mean steady-state plasma concentrations of labetalol in patients undergoing antihypertensive therapy. British Journal of Clinical Pharmacology 8: 153S–155S (1979).
Tarazi, R.C. and Dunstan, H.P.: Beta adrenergic blockade in hypertension. American Journal of Cardiology 29: 633–640 (1972).
Thompson, F.D.; Joekes, A.M. and Hussein, M.M.: Labetalol used as a hypotensive agent in the presence of renal disease. Kidney International 11 (4): 287–288 (1977).
Walstad, R.A.; Nilsen, O.G.; Berg, K.J. and Wessel-Aas, T.: The pharmacokinetics and clinical effect of one single dose of labetalol in patients with normal and impaired renal function. Acta Pharmacologica et Toxicologica 49: 54 (1981).
Wilkinson, G.R.: Pharmacokinetics in disease states modifying body perfusion; in Benet (Ed.) The Effect of Disease States on Drug Pharmacokinetics, pp. 13–32 (American Pharmaceutical Association, Washington DC 1976).
Wood, A.J.; Ferry, D.G. and Bailey, R.R.: Elimination kinetics of labetalol in severe renal failure. British Journal of Clinical Pharmacology 13 (Suppl. 1): 81S–86S (1982).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
McNeil, J.J., Louis, W.J. Clinical Pharmacokinetics of Labetalol. Clin Pharmacokinet 9, 157–167 (1984). https://doi.org/10.2165/00003088-198409020-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-198409020-00003