Abstract
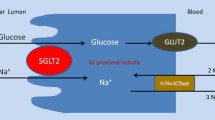
The kidney plays a major role in glucose homeostasis because of its role in gluconeogenesis and the glomerular filtration and reabsorption of glucose in the proximal convoluted tubules. Approximately 180 g of glucose is filtered daily in the glomeruli of a normal healthy adult. Typically, all of this glucose is reabsorbed with <1% being excreted in the urine. The transport of glucose from the tubule into the tubular epithelial cells is accomplished by sodium-glucose co-transporters (SGLTs). SGLTs encompass a family of membrane proteins that are responsible for the transport of glucose, amino acids, vitamins, ions and osmolytes across the brush-border membrane of proximal renal tubules as well as the intestinal epithelium. SGLT2 is a high-capacity, low-affinity transporter expressed chiefly in the kidney. It accounts for approximately 90% of glucose reabsorption in the kidney and has thus become the focus of a great deal of interest in the field of diabetes mellitus.
SGLT2 inhibitors block the reabsorption of filtered glucose leading to glucosuria. This mechanism of action holds potential promise for patients with type 2 diabetes mellitus (T2DM) in terms of improvements in glycaemic control. In addition, the glucosuria associated with SGLT2 inhibition is associated with caloric loss, thus providing a potential benefit of weight loss. Dapagliflozin is the SGLT2 inhibitor with the most clinical data available to date, with other SGLT2 inhibitors currently in the developmental pipeline. Dapagliflozin has demonstrated sustained, dose-dependent glucosuria over 24 hours with once-daily dosing in clinical trials. Although long-term safety data are lacking, studies to date have generally found dapagliflozin to be safe and well tolerated. Concerns related to SGLT2 inhibition include the fact that by their very nature they cause glucose elevation in the urine that can theoretically lead to urinary tract and genital infections, electrolyte imbalances and increased urinary frequency. Although studies to date have been promising in terms of these and other concerns, longer-term studies evaluating the usual safety and efficacy outcomes will need to be conducted. Similarly, head-to-head comparator trials are needed to determine the role of SGLT2 inhibitors in relation to the many other therapeutic options available for the treatment of T2DM. If significant reductions in haemoglobin Alc are associated with SGLT2 inhibitor therapy, and these agents are determined to be safe and well tolerated in the long term, they could become a major breakthrough in the T2DM treatment armamentarium.

Similar content being viewed by others
References
American Diabetes Association. All about diabetes [online]. Available from URL: http://www.diabetes.org/about-diabetes.jsp [Accessed 2009 Oct 10]
Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2007. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2008
Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008; 358: 2560–72
Moss SE, Klein R, Klein BE, et al. The association of glycemia and cause specific mortality in a diabetic population. Arch Intern Med 1994; 154: 2473–9
Ray KK, Seshasai SR, Wijesuriya S, et al. Effect of intensive control of glucose on cardiovascular outcomes and death in patients with diabetes mellitus: a meta-analysis of randomised controlled trials. Lancet 2009; 373: 1765–72
Ong KL, Cheung BM, Wong LY, et al. Prevalence, treatment and control of diagnosed diabetes in the U.S. National Health and Nutrition Examination Survey 1999-2004. Ann Epidemiol 2008; 18: 222–9
Wani JH, John-Kalarickal J, Fonseca VA. Dipeptidyl peptidase-4 as a new target of action for type 2 diabetes mellitus: a systematic review. Cardiol Clin 2008; 26: 639–48
Resnick HE, Foster GL, Bardsley J, et al. Achievement of American Diabetes Association clinical practice recommendations among U.S. adults with diabetes, 1999-2002: the National Health and Nutrition Examination Survey. Diabetes Care 2006; 29: 531–7
U.K. Prospective Diabetes Study Group. U.K. prospective diabetes study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes 1995; 44: 1249–58
Turner RC, Cull CA, Frighi V, et al. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA 1999; 281: 2005–12
Wright EM, Turk E. The sodium/glucose cotransport family SLC 5. Eur J Physiol 2004; 447: 510–8
Kanai Y, Lee W-S, You G, et al. The human kidney low affinity Na+/glucose cotransporter SGLT 2. J Clin Invest 1994; 93: 397–404
Asano T, Anai M, Sakoda H, et al. SGLT as a therapeutic target. Drugs Fut 2004; 29: 461–6
Asano T, Ogihara T, Katagiri H, et al. Glucose cotransporter and Na+/glucose cotransporter as molecular targets of anti-diabetic drugs. Curr Med Chem 2004; 11: 2717–24
Gerich JE, Woerle HJ, Meyer C, et al. Renal gluconeogenesis. Diabetes Care 2001; 24(2): 382–91
Guyton AC, Hall JE. Textbook of medical physiology. 9th ed. Philadelphia (PA): W.B. Saunders Company, 1996: 31
Gullans SR. Metabolic basis of solute transport. In: Brenner BM, editor. Brenner and Rector’s, the kidney. 6th ed. Philadelphia (PA): W.B. Saunders Company, 2000: 234–5
Stumvoll M, Meyer C, Mitrakou A, et al. Renal glucose production and utilization: new aspects in humans. Diabetologia 1997; 40: 749–57
Meyer C, Stumvoll M, Nadkarni V, et al. Abnormal renal and hepatic glucose metabolism in type 2 diabetes mellitus. J Clin Invest 1998; 102: 619–24
Guyton AC, Hall JE. Textbook of medical physiology. 9th ed. Philadelphia (PA): W.B. Saunders Company, 1996: 332–5
Wright EM. Renal N+-glucose transporters. Am J Physiol Renal Physiol 2001; 280: F10–8
Butterfield WJH, Keen H, Whichelow MJ. Renal glucose threshold variations with age. BMJ 1967; 4: 505–7
Moe OW, Berry CA, Rector FC. Renal transport of glucose, amino acids, sodium, chloride, and water. In: Brenner BM, editor. Brenner and Rector’s, the kidney. 6th ed. Philadelphia (PA): W.B. Saunders Company, 2000: 378–80
Bakris GL, Fonseca V, Sharma K, et al. Renal sodium-glucose transport: role in diabetes mellitus and potential clinical implications. Kidney International 2009; 75: 1272–7
Wright EM, Hirayama BA, Loo DF. Active sugar transport in health and disease. J Intern Med 2007; 261: 32–43
Abdul-Ghani MA, DeFronzo R. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocrine Practice 2008; 14(6): 782–90
Stumvoll M, Chintalapudi U, Perriello G, et al. Uptake and release of glucose by the human kidney: postabsorptive rates and responses to epinephrine. J Clin Invest 1995; 96: 2528–33
Meyer C, Dostou JM, Welle L, et al. Role of human liver, kidney, and skeletal muscle in postprandial glucose homeostasis. Am J Physiol Endocrinol Met 2002; 282: E419–27
Ehrenkranz RRL, Lewis NG, Kahn CR, et al. Phlorizin: a review. Diabetes Metab Res Rev 2005; 21: 31–8
Dudash Jr J, Zhang X, Zeck RE, et al. Glycosylated dihydrochalcones as potent and selective sodium glucose co-transporters 2 (SGLT2) inhibitors. Bioorg Med Chem Lett 2004; 14: 5121–5
Chassis H, Joliffe N, Smith H. The action of phlorizin on the excretion of glucose, xylose, sucrose, creatinine and urea by man. J Clin Invest 1933; 12: 1083–9
Lee WS, Wells RG, Hediger MA. The high affinity NA/glucose cotransporter: re-evaluation and distribution of expression. J Biol Chem 1994; 269: 12032–9
Idris I, Donnelly R. Sodium-glucose co-transporter-2 inhibitors: an emerging new class of oral antidiabetic drug. Diabetes Obes Metab 2009; 11: 79–88
List JF, Woo V, Morales E, et al. Sodium-glucose cotrans-port inhibition with dapagliflozin in type 2 diabetes. Diabetes Care 2009; 32: 650–7
Marsenic O. Glucose control by the kidney: an emerging target in diabetes. Am J Kidney Dis 2009; 53: 875–83
Jabbour SA, Goldstein BJ. Sodium glucose co-transporter 2 inhibitors: blocking renal tubular re-absorption of glucose to improve glycaemic control in patients with diabetes. Int J Clin Pract 2008; 62: 1279–84
Komoroski B, Vachharajani N, Boulton D, et al. Dapagliflozin, a novel SGLT2 inhibitor, induces dose-dependent glucosuria in healthy subjects. Clin Pharm Ther 2009; 85: 520–4
Komoroski B, Vachharajani N, Feng Y, et al. Dapagliflozin, a novel, selective SGLT2 inhibitor, improved glycemic control over 2 weeks in patients with type 2 diabetes mellitus. Clin Pharm Ther 2009; 85: 513–9
Bailey CJ, Gross JL, Bastone L, et al. Dapagliflozin as an add-on to metformin lowers hyperglycemia in type 2 diabetes patients inadequately controlled with metformin alone [abstract no. OP169]. Diabetologia 2009; 52 Suppl. 1: S76
Wilding JPH, Norwood P, T’joen C, et al. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers. Diabetes Care 2009; 32: 1656–62
US National Institutes of Health. ClinicalTrials.gov [online]. Available from URL: http://www.clinicaltrials.gov [Accessed 2009 Oct 10]
Lesli B, Tang W, List JF. Renal effects of the sodium-glucose co-transporter 2 (SGLT2) inhibitor depagliflozin (BMS-512148) in patients with type 2 diabetes mellitus (T2DM) [abstract no. PO1022]. J Am Soc Nephrol 2008; 19
Kissei Pharmaceutical Co., Ltd. Discontinuation of the development of “Remogliflozin” by GlaxoSmithKline [online]. Available from URL: http://www.kissei.co.fp/e_contents/press_e/2009/e20090703.html [Accessed 2009 Oct 10]
Colca JR. Discontinued drugs in 2008: endocrine and metabolic. Exp Opin Invest Drugs 2009; 18: 1243–55
Adachi T, Yasuda K, Okamoto Y, et al. T-1095, a renal Na+-glucose transporter inhibitor, improves hyperglycemia in streptozotocin-induced diabetic rats. Metabolism 2000; 49: 990–5
Katsuno K, Fujimori Y, Takemura Y, et al. Sergliflozin, a novel selective inhibitor of low-affinity sodium glucosa cotransporter (SGLT2), validates the critical role of SGLT2 in renal glucose reabsorption and modulates plasma glucose level. J Pharmacol Exp Ther 2007; 320: 323–30
Han S, Hagan DL, Taylor JR, et al. Dapagliflozin, a selective SGLT2 inhibitor, improves glucose homeostasis in normal and diabetic rats. Diabetes 2008; 57: 1723–9
Fujimori Y, Katsuno K, Nakashima I, et al. Remogliflozin etabonate, in a novel category of selective low-affinity sodium glucose cotransporter (SGLT2) inhibitors, exhibits antidiabetic efficacy in rodent models. J Pharmacol Exp Ther 2008; 327: 268–76
Meng W, Ellsworth BA, Nirschl AA, et al. Discovery of dapagliflozin: a potent, selective renal sodium-dependent glucose cotransporter 2 (SGLT2) inhibitor for the treatment of type 2 diabetes. J Med Chem 2008; 51: 1145–9
Acknowledgements
No sources of funding support were utilized to assist in the preparation of this article. None of the authors report conflicts of interest that are directly related to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neumiller, J.J., White, J.R. & Campbell, R.K. Sodium-Glucose Co-Transport Inhibitors. Drugs 70, 377–385 (2010). https://doi.org/10.2165/11318680-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11318680-000000000-00000